Monday Poster Session
Category: Functional Bowel Disease
P2333 - Bias in the Bowel: Disparities in Diagnostic Testing for Constipation
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ahmun Zafar, DO
Mount Sinai West, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Ahmun Zafar, DO1, Joseph Menand, MD1, Yuying Luo, MD2
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai Center for Gastrointestinal Physiology & Motility, New York, NY
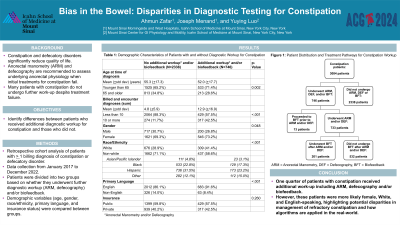
Introduction: Constipation and defecatory disorders significantly impact patients' quality of life. Diagnostic procedures such as anorectal manometry (ARM) and defecography, are recommended to evaluate underlying anorectal physiology when initial treatments for constipation fail, although many patients do not undergo further work-up. We aim to identify patient-level differences between those who underwent further diagnostic workup for constipation and those who did not.
Methods: We conducted a retrospective cohort analysis of patients with at least one billing diagnosis of constipation or defecatory disorders at one tertiary academic clinic with onsite access to ARM and defecography from January 2017 to December 2022. Patients were divided into two groups based on whether they underwent further diagnostic workup (ARM, defecography) and/or biofeedback. Demographic variables, including age, gender, race, primary language, and insurance status, were compared between groups.
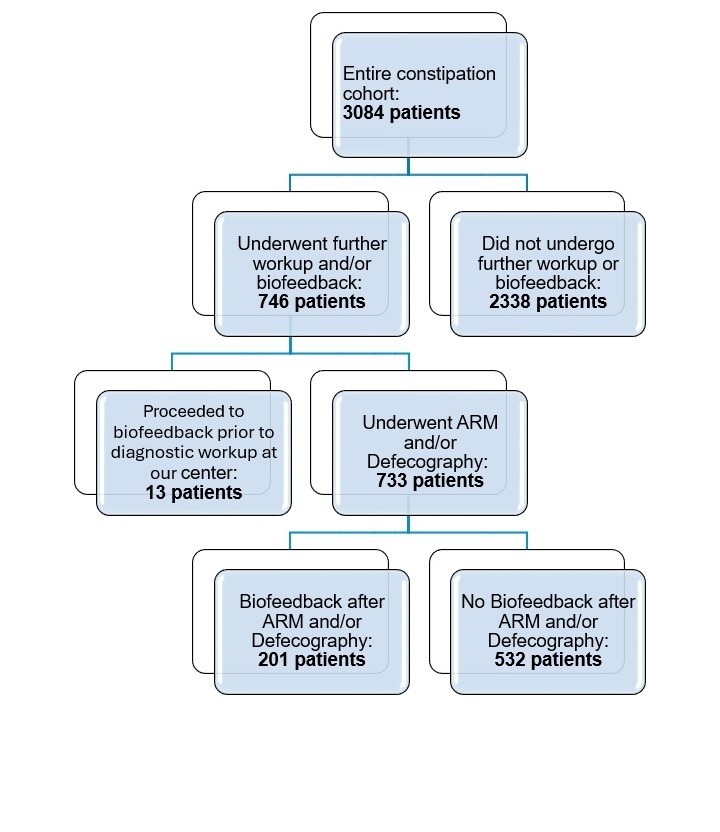
Results: Our entire cohort included 3084 patients, with average age 54.5 + 17.4 (66.7% younger than 65), 70.3% female, 31.9% white and 86.7% English speaking. 24.2% of patients underwent ARM, defecography and/or biofeedback for constipation. Patients who underwent additional workup and/or biofeedback for constipation were more likely female (73.2% vs. 26.8%, p=0.048), white (41.3% vs. 58.7%, p< 0.001), and English-speaking (90.6% vs 9.4%, p< 0.001). Patients with ten or more billing and/or encounter diagnoses for constipation were significantly more likely to have undergone further workup and/or biofeedback than patients with less than ten constipation diagnoses (42.5% vs 57.5%, p< 0.001) (Table 1). Of the 733 patients who underwent ARM and/or defecography, 201 (27.4%) went on to get biofeedback (Figure 1).
Discussion: One quarter of patients with constipation at one tertiary center with onsite access to ARM received additional work-up including ARM, defecography and/or biofeedback, higher than previously reported in the literature. However, these patients were more likely female, white, and English-speaking, highlighting potential disparities in management of refractory constipation and how algorithms are applied in the real-world.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ahmun Zafar, DO1, Joseph Menand, MD1, Yuying Luo, MD2. P2333 - Bias in the Bowel: Disparities in Diagnostic Testing for Constipation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai Center for Gastrointestinal Physiology & Motility, New York, NY
Introduction: Constipation and defecatory disorders significantly impact patients' quality of life. Diagnostic procedures such as anorectal manometry (ARM) and defecography, are recommended to evaluate underlying anorectal physiology when initial treatments for constipation fail, although many patients do not undergo further work-up. We aim to identify patient-level differences between those who underwent further diagnostic workup for constipation and those who did not.
Methods: We conducted a retrospective cohort analysis of patients with at least one billing diagnosis of constipation or defecatory disorders at one tertiary academic clinic with onsite access to ARM and defecography from January 2017 to December 2022. Patients were divided into two groups based on whether they underwent further diagnostic workup (ARM, defecography) and/or biofeedback. Demographic variables, including age, gender, race, primary language, and insurance status, were compared between groups.
Results: Our entire cohort included 3084 patients, with average age 54.5 + 17.4 (66.7% younger than 65), 70.3% female, 31.9% white and 86.7% English speaking. 24.2% of patients underwent ARM, defecography and/or biofeedback for constipation. Patients who underwent additional workup and/or biofeedback for constipation were more likely female (73.2% vs. 26.8%, p=0.048), white (41.3% vs. 58.7%, p< 0.001), and English-speaking (90.6% vs 9.4%, p< 0.001). Patients with ten or more billing and/or encounter diagnoses for constipation were significantly more likely to have undergone further workup and/or biofeedback than patients with less than ten constipation diagnoses (42.5% vs 57.5%, p< 0.001) (Table 1). Of the 733 patients who underwent ARM and/or defecography, 201 (27.4%) went on to get biofeedback (Figure 1).
Discussion: One quarter of patients with constipation at one tertiary center with onsite access to ARM received additional work-up including ARM, defecography and/or biofeedback, higher than previously reported in the literature. However, these patients were more likely female, white, and English-speaking, highlighting potential disparities in management of refractory constipation and how algorithms are applied in the real-world.
Figure: Patient Distribution and Treatment Pathways for Constipation Workup
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ahmun Zafar indicated no relevant financial relationships.
Joseph Menand indicated no relevant financial relationships.
Yuying Luo indicated no relevant financial relationships.
Ahmun Zafar, DO1, Joseph Menand, MD1, Yuying Luo, MD2. P2333 - Bias in the Bowel: Disparities in Diagnostic Testing for Constipation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
