Monday Poster Session
Category: Functional Bowel Disease
P2337 - Baseline Severity Correlates with Symptom Improvement on Novel Digital Hypnotherapy Intervention for Bloating
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Xiao Jing Wang, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Xiao Jing (Iris) Wang, MD1, Anjali Rajagopal, MBBS1, Saam Dilmaghani, MD, MPH1, Mauricio Jin, MD1, Conor Loftus, MD1, Lindsey Philpot, PhD, MPH1, Jon Ebbert, MD1, Olafur Palsson, PhD2
1Mayo Clinic, Rochester, MN; 2University of North Carolina, Chapel Hill, NC
Introduction: Abdominal bloating alone or as part of another disorder of gut brain interaction is difficult to treat. Hypnotherapy and diaphragmatic breathing have separately shown benefits in prior work but have not been united in a single intervention. We recently reported (Gastroenterology 2024, 166(5) Suppl: S491–S-492) that a study of a novel self-guided protocol integrating hypnosis and diaphragmatic breathing showed significant improvement in bloating as well as other bowel symptoms. In this follow up, we performed subgroup analysis to understand the impact of baseline symptoms on treatment response.
Methods: Patients with non-organic bowel disorders with predominant bloating symptoms completed the 7-session hypnotherapy program via a digital app. Patients completed symptom (IBS-SSS, PAGI-SYM), visceral sensitivity index (VSI)), and quality of life (QoL) (EuroQuol-5d (EQ5D)) assessments at baseline, end-of-treatment and 3-month follow-up. Subgroup analysis was performed by baseline symptom severity utilizing ANOVA or t-test.
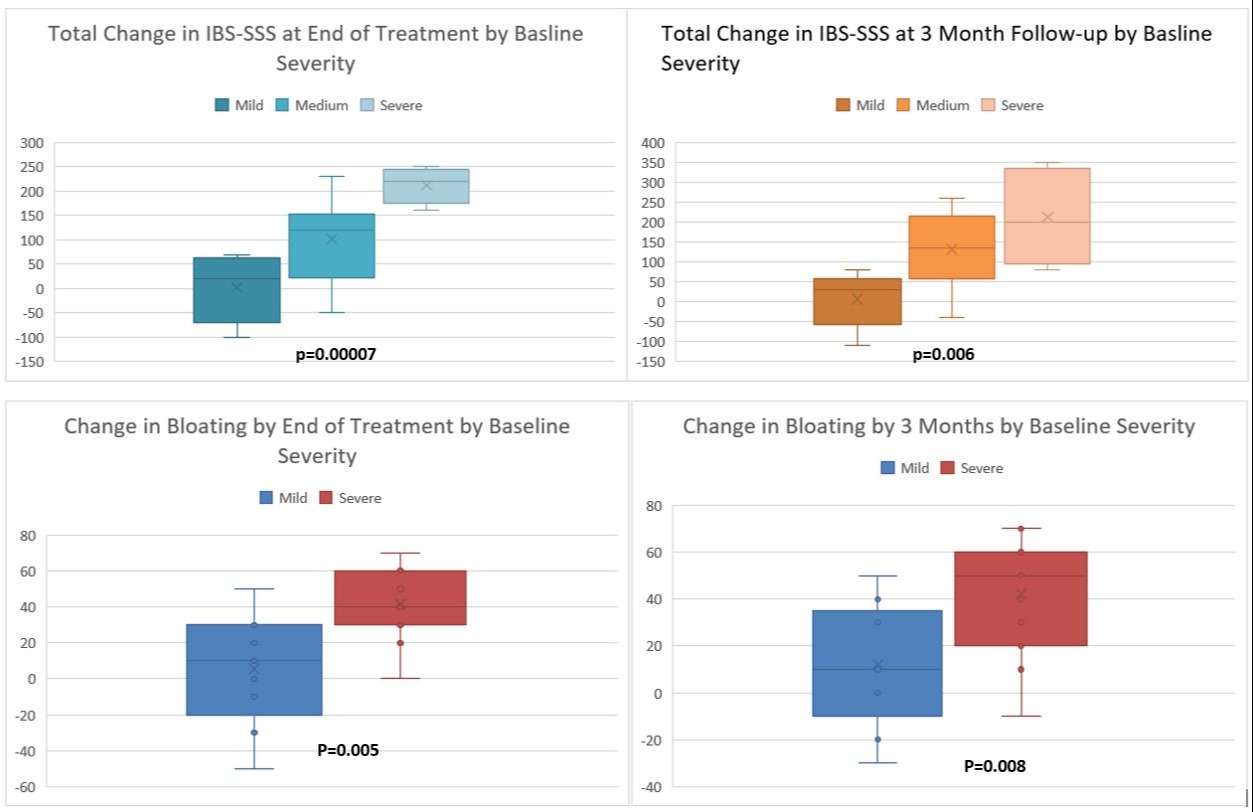
Results: 22 of 23 (95.6%) patients completed treatment and follow up with significant improvements on IBS-SSS total severity and bloating scores (primary outcome), PAGI-SYM, and symptom specific anxiety (VSI) with large effect sizes at end of treatment and 3 month follow up with 73.9% showing >30% improvement in total IBS-SSS. <br>In subgroup analysis, those with severe baseline IBS showed greater improvement compared to moderate and mild groups at end of treatment (p=0.00007) and 3 month follow up (p=0.006). Patients with high ( >50) baseline bloating scores had larger improvement in bloating than those with lower (< 50) scores (p=0.005) (Figure 1). <br>Baseline severity was not significantly correlated with baseline QOL or VSI. Mean improvement in QoL at 3 month follow up was numerically but not significantly (p=0.48) greater in those with severe baseline IBS-SSS (12.8 vs 2.33, -8.25 in mild, moderate) Improvement in VSI was similarly greater with more severity but nonsignificant (Table 1).
Discussion: Our novel digital intervention showed improvement in symptom burden as well as symptoms specific anxiety. Subgroup analysis shows that greater baseline IBS-SSS severity was associated with larger response to treatment but not with symptom specific anxiety or quality of life, suggesting factors beyond symptom severity. Further randomized controlled trials are currently planned.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Xiao Jing (Iris) Wang, MD1, Anjali Rajagopal, MBBS1, Saam Dilmaghani, MD, MPH1, Mauricio Jin, MD1, Conor Loftus, MD1, Lindsey Philpot, PhD, MPH1, Jon Ebbert, MD1, Olafur Palsson, PhD2. P2337 - Baseline Severity Correlates with Symptom Improvement on Novel Digital Hypnotherapy Intervention for Bloating, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2University of North Carolina, Chapel Hill, NC
Introduction: Abdominal bloating alone or as part of another disorder of gut brain interaction is difficult to treat. Hypnotherapy and diaphragmatic breathing have separately shown benefits in prior work but have not been united in a single intervention. We recently reported (Gastroenterology 2024, 166(5) Suppl: S491–S-492) that a study of a novel self-guided protocol integrating hypnosis and diaphragmatic breathing showed significant improvement in bloating as well as other bowel symptoms. In this follow up, we performed subgroup analysis to understand the impact of baseline symptoms on treatment response.
Methods: Patients with non-organic bowel disorders with predominant bloating symptoms completed the 7-session hypnotherapy program via a digital app. Patients completed symptom (IBS-SSS, PAGI-SYM), visceral sensitivity index (VSI)), and quality of life (QoL) (EuroQuol-5d (EQ5D)) assessments at baseline, end-of-treatment and 3-month follow-up. Subgroup analysis was performed by baseline symptom severity utilizing ANOVA or t-test.
Results: 22 of 23 (95.6%) patients completed treatment and follow up with significant improvements on IBS-SSS total severity and bloating scores (primary outcome), PAGI-SYM, and symptom specific anxiety (VSI) with large effect sizes at end of treatment and 3 month follow up with 73.9% showing >30% improvement in total IBS-SSS. <br>In subgroup analysis, those with severe baseline IBS showed greater improvement compared to moderate and mild groups at end of treatment (p=0.00007) and 3 month follow up (p=0.006). Patients with high ( >50) baseline bloating scores had larger improvement in bloating than those with lower (< 50) scores (p=0.005) (Figure 1). <br>Baseline severity was not significantly correlated with baseline QOL or VSI. Mean improvement in QoL at 3 month follow up was numerically but not significantly (p=0.48) greater in those with severe baseline IBS-SSS (12.8 vs 2.33, -8.25 in mild, moderate) Improvement in VSI was similarly greater with more severity but nonsignificant (Table 1).
Discussion: Our novel digital intervention showed improvement in symptom burden as well as symptoms specific anxiety. Subgroup analysis shows that greater baseline IBS-SSS severity was associated with larger response to treatment but not with symptom specific anxiety or quality of life, suggesting factors beyond symptom severity. Further randomized controlled trials are currently planned.
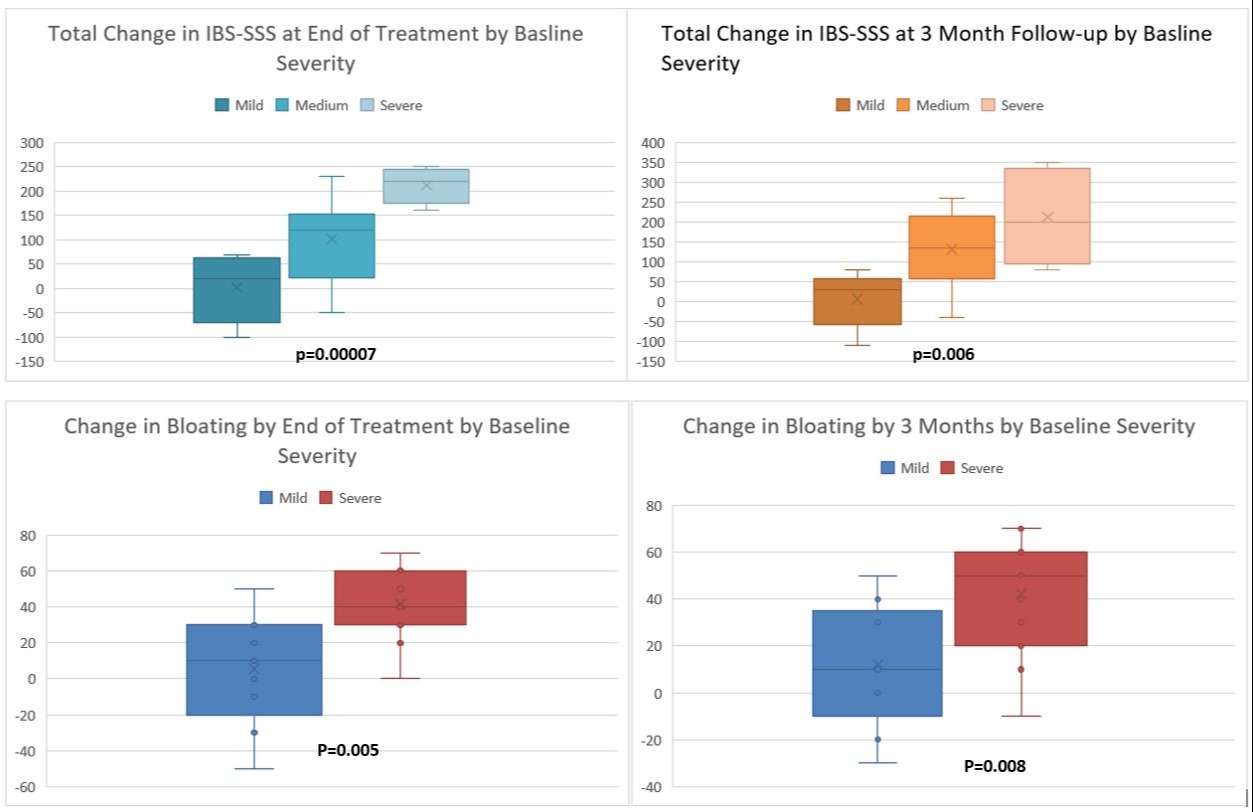
Figure: Change in IBS-SSS and IBS-bloating subscores stratified by baseline severity at end of treatment and 3 month follow up.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Xiao Jing (Iris) Wang indicated no relevant financial relationships.
Anjali Rajagopal indicated no relevant financial relationships.
Saam Dilmaghani indicated no relevant financial relationships.
Mauricio Jin indicated no relevant financial relationships.
Conor Loftus indicated no relevant financial relationships.
Lindsey Philpot indicated no relevant financial relationships.
Jon Ebbert: Alnylam – Consultant. Applied Aerosol Technologies – Royalties. Exact Sciences – Advisory Committee/Board Member, Speakers Bureau. Lin Health – Royalties.
Olafur Palsson indicated no relevant financial relationships.
Xiao Jing (Iris) Wang, MD1, Anjali Rajagopal, MBBS1, Saam Dilmaghani, MD, MPH1, Mauricio Jin, MD1, Conor Loftus, MD1, Lindsey Philpot, PhD, MPH1, Jon Ebbert, MD1, Olafur Palsson, PhD2. P2337 - Baseline Severity Correlates with Symptom Improvement on Novel Digital Hypnotherapy Intervention for Bloating, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
