Monday Poster Session
Category: Functional Bowel Disease
P2338 - Utilization of Bowel Regimens in the Medical Intensive Care Unit
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Christopher J. Costa, MD
University of Connecticut Health Center
Farmington, CT
Presenting Author(s)
Christopher J. Costa, MD1, Rachael Hagen, DO2, Raymond Foley, DO2
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut Health, Farmington, CT
Introduction: Recent work has shown that up to 72% of patients admitted to the intensive care unit (ICU) experience Impaired GI Transit (IGT) during their stay, associated with increased morbidity and mortality. Prophylactic dosing of laxatives is superior to treatment dosing. We analyzed the use of laxatives in the medical intensive care unit (MICU) in an academic hospital to determine patterns of use among clinicians.
Methods: Records of patients admitted to the MICU for a 6-month period were reviewed for age, sex, admitting diagnosis, bowel regimen, time to first bowel movement (BM), and use of vasopressors. Statistical analysis included Χ2 testing of bowel regimen agents and comparison of means with Student’s t Test. ICU-associated IGT was defined as >72h from admission without BM. This work was granted exempt status by UConn Health IRB: 24X-008-2.
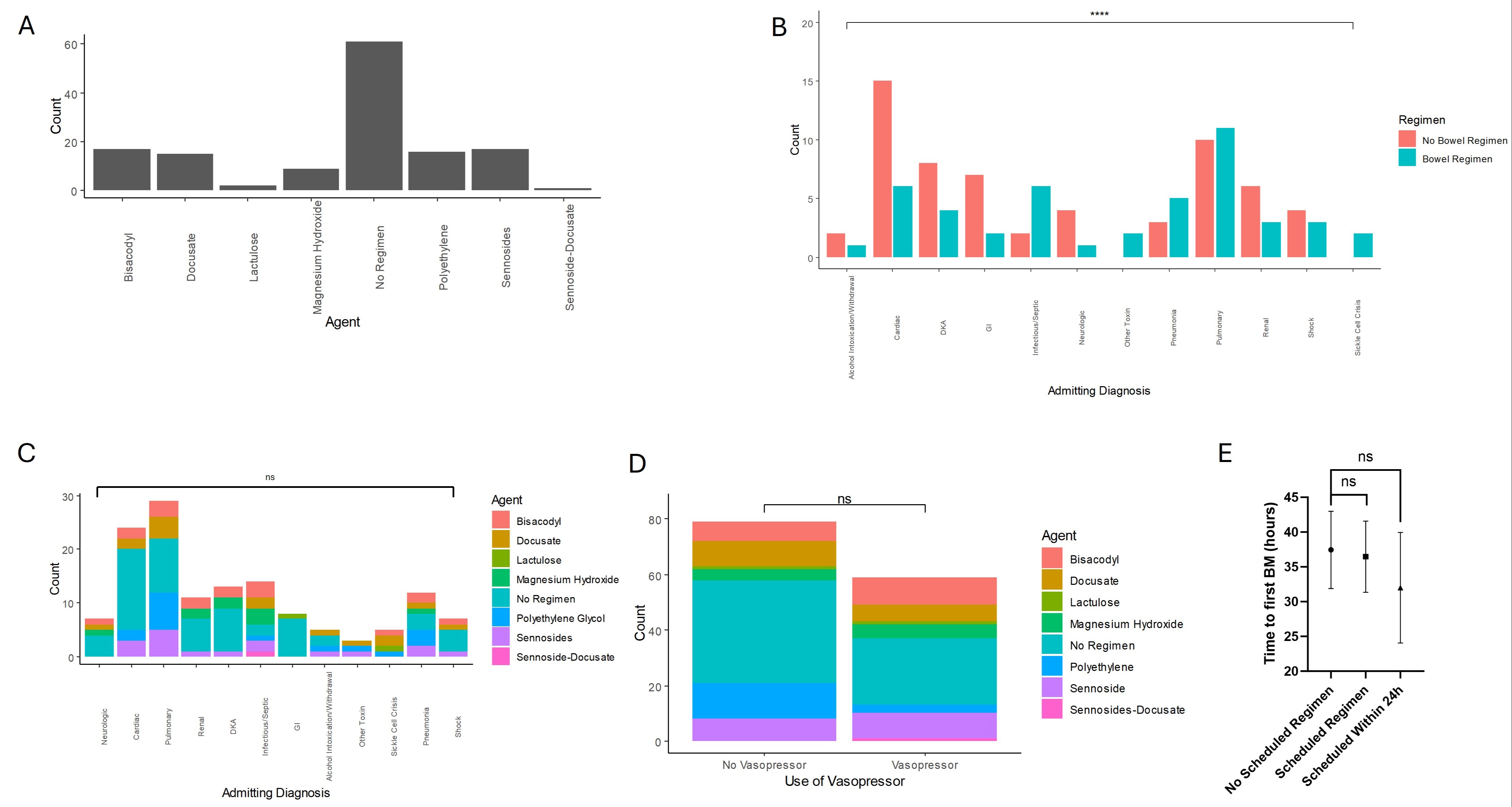
Results: 107 charts were reviewed. Patients were mostly male (n=63, 58.9%) with a mean age of 63 (σ=21), with admission diagnosis involving cardiac (n=21, 19.6%) or pulmonary (n=21, 19.6%) systems (Table 1). 49 (45.8%) were receiving vasopressors and 30 (28%) were receiving opioid infusions. Median length of stay was 47.4 h (IQR 70.9 h). Only 39 (36.4%) patients had a scheduled bowel regimen, with only 15 receiving any agent within the first 24 hours. Sennosides and bisacodyl were the most common agents (both n=17, 15.9%) (Figure 1A). There were significant differences in regimen use by admitting diagnosis (Χ2=23.4, df=11, p=0.02), however, agent of choice did not differ (Χ2=84.4, df=66, p=0.06) (Figure 1B&C). Notably, cardiac admitting diagnoses were the greatest number without a bowel regimen ordered on admission, which was statistically significant (Χ2=41.9, df=11, p=1.7e-05). Scheduled bowel regimen did not differ by use of vasopressor (Χ2=1.8, df=1, p=0.18) (Figure 1D). While the mean time to first BM was shorter for patients with scheduled regimens and even shorter for those receiving an agent within the first 24 hours (Figure 1E), these differences were not statistically significant.
Discussion: Prescribing practices at our single center show a reactive approach to ICU-associated IGT, with few patients placed on a prophylactic regimen. Part of this prescribing practice seems to be due to admitting diagnosis, reflective of clinician predicted length of stay and severity of illness. Our work suggests that at our facility, and likely many others, ICU-associated IGT incidence and its treatment is an underappreciated entity requiring further study.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Christopher J. Costa, MD1, Rachael Hagen, DO2, Raymond Foley, DO2. P2338 - Utilization of Bowel Regimens in the Medical Intensive Care Unit, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut Health, Farmington, CT
Introduction: Recent work has shown that up to 72% of patients admitted to the intensive care unit (ICU) experience Impaired GI Transit (IGT) during their stay, associated with increased morbidity and mortality. Prophylactic dosing of laxatives is superior to treatment dosing. We analyzed the use of laxatives in the medical intensive care unit (MICU) in an academic hospital to determine patterns of use among clinicians.
Methods: Records of patients admitted to the MICU for a 6-month period were reviewed for age, sex, admitting diagnosis, bowel regimen, time to first bowel movement (BM), and use of vasopressors. Statistical analysis included Χ2 testing of bowel regimen agents and comparison of means with Student’s t Test. ICU-associated IGT was defined as >72h from admission without BM. This work was granted exempt status by UConn Health IRB: 24X-008-2.
Results: 107 charts were reviewed. Patients were mostly male (n=63, 58.9%) with a mean age of 63 (σ=21), with admission diagnosis involving cardiac (n=21, 19.6%) or pulmonary (n=21, 19.6%) systems (Table 1). 49 (45.8%) were receiving vasopressors and 30 (28%) were receiving opioid infusions. Median length of stay was 47.4 h (IQR 70.9 h). Only 39 (36.4%) patients had a scheduled bowel regimen, with only 15 receiving any agent within the first 24 hours. Sennosides and bisacodyl were the most common agents (both n=17, 15.9%) (Figure 1A). There were significant differences in regimen use by admitting diagnosis (Χ2=23.4, df=11, p=0.02), however, agent of choice did not differ (Χ2=84.4, df=66, p=0.06) (Figure 1B&C). Notably, cardiac admitting diagnoses were the greatest number without a bowel regimen ordered on admission, which was statistically significant (Χ2=41.9, df=11, p=1.7e-05). Scheduled bowel regimen did not differ by use of vasopressor (Χ2=1.8, df=1, p=0.18) (Figure 1D). While the mean time to first BM was shorter for patients with scheduled regimens and even shorter for those receiving an agent within the first 24 hours (Figure 1E), these differences were not statistically significant.
Discussion: Prescribing practices at our single center show a reactive approach to ICU-associated IGT, with few patients placed on a prophylactic regimen. Part of this prescribing practice seems to be due to admitting diagnosis, reflective of clinician predicted length of stay and severity of illness. Our work suggests that at our facility, and likely many others, ICU-associated IGT incidence and its treatment is an underappreciated entity requiring further study.
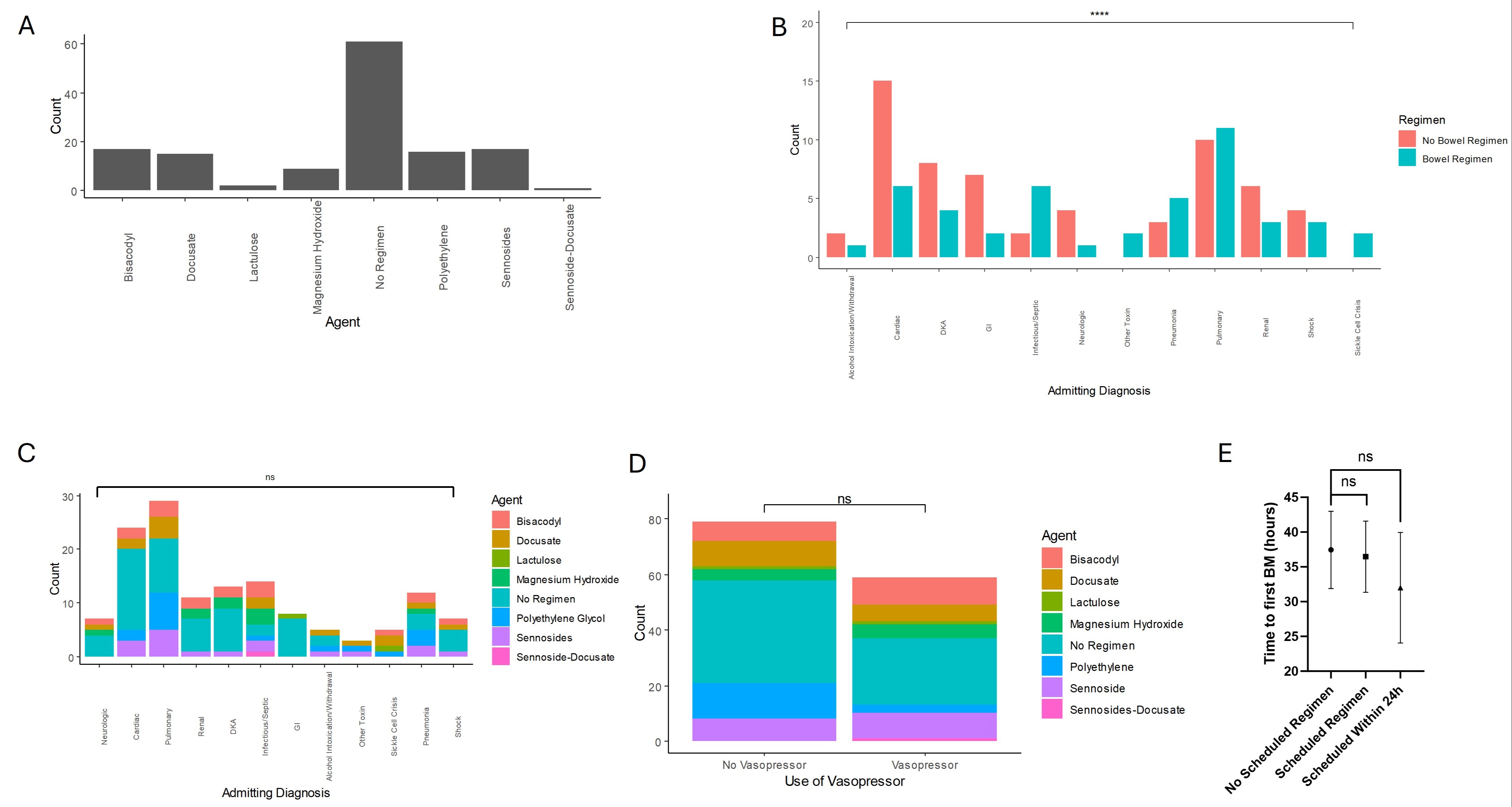
Figure: Figure 1: (A) Laxative agent of choice in the MICU favored stimulant laxatives with Sennosides and Bisacodyl being the most common. (B) Use of regimen differed significantly dependent on admitting diagnosis, with cardiac diagnoses being most likely to not have a scheduled regimen, however, (C) there were no significant differences in choice of regimen by diagnosis. (D) Vasopressor use was not associated with any significant differences in choice or utilization of a bowel regimen. (E) While there are trends towards a shorter time to first bowel movement with scheduled regimen, especially when given within 24 hours of admission, these differences were not significant. (****) p<0.0001
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Christopher Costa indicated no relevant financial relationships.
Rachael Hagen indicated no relevant financial relationships.
Raymond Foley indicated no relevant financial relationships.
Christopher J. Costa, MD1, Rachael Hagen, DO2, Raymond Foley, DO2. P2338 - Utilization of Bowel Regimens in the Medical Intensive Care Unit, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
