Monday Poster Session
Category: Functional Bowel Disease
P2339 - Correlation of Point-of-Care, Digital Signal Processed, Bowel Sounds With Lactulose Breath Testing in Patients With Irritable Bowel Syndrome
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Sachin N. Mysore, BA
EndoLogic, NJ
Presenting Author(s)
Sachin N. Mysore, BA1, Zahf Shaikh, DO2, Shiv Patel, BS3, Neel Godbole, 4, Zamir S. Brelvi, MD, PhD5, Sourav Dutta, MD6
1EndoLogic, Edison, NJ; 2Hackensack University Medical Center, Randolph, NJ; 3Endologic LLC, Parsippany, NJ; 4Brown University, Parsippany, NJ; 5Endologic LLC, Montville, NJ; 6Endologic, Franklin Lakes, NJ
Introduction: Irritable Bowel Syndrome (IBS) is a functional motility disorder characterized by abdominal pain, bloating, and abnormal stool. Our previous study demonstrated that bowel sound analysis (BSA) correlates with symptom severity in patients with IBS. In this study, we develop a model to identify bowel sound events (BSEs) and analyze how bowel sound scores (BS) are associated with IBS symptom severity and Lactulose breath testing (LBT) in an outpatient clinical setting. Digital Signal Processing (DSP) provides a tool to quantify and study BS in motility disorders like IBS.
Methods: This retrospective case-control study includes IBS patients who met Rome IV criteria. Patients completed the Gastrointestinal Symptom Rating Scale (GSRS-IBS) pre-appointment. A score ≥35 was considered an IBS flare-up. BS were recorded from 3 points 4 cm left, right, and below the umbilicus for 15 seconds each with an electronic stethoscope. BSEs were identified using a proprietary algorithm that uses proven DSP methods relating to time and frequency analysis. BSEs were characterized by a BSA score, whose value increases with the number of detected events, and the duration between BSEs. Patients received TrioSmart LBT (Gemelli Biotech) to complete post-appointment.
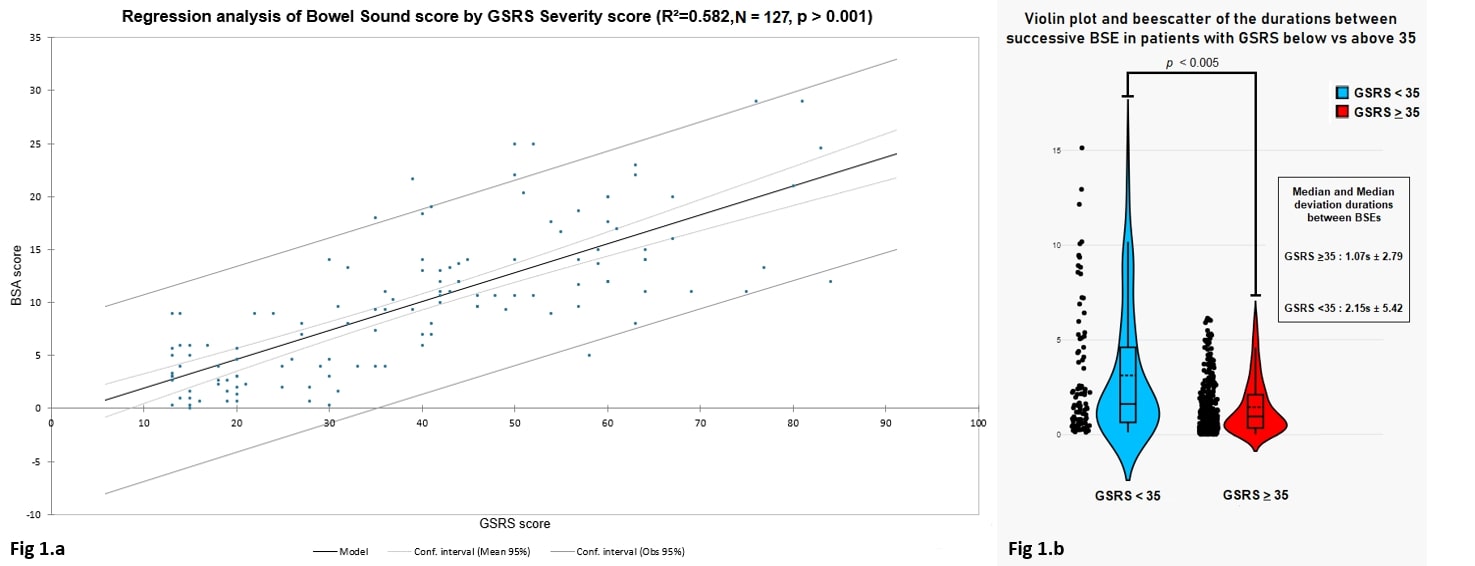
Results: 127 patients meeting Rome IV criteria were evaluated with the GSRS, yielding 74 patients with active flare-ups (GSRS ≥35) and 53 patients in a symptomatically quiescent state (GSRS < 35). Comparing symptom scores with the BSA scores yielded a scatterplot with an R2 = 0.582 and an ANOVA of regression yielding a p< 0.001 (1.a.). The scatterplot shows a cutoff BS score of 8.5. This yields 72 patients with active flare-ups (BSA ≥8.5) and 55 in a symptomatically quiescent state (BSA < 8.5).
Analyzing the duration between BSEs, patients with GSRS ≥35 had a median duration of 1.07 seconds vs 2.15 seconds for patients < 35. A Pearson’s R test between both sets yields a p< 0.005 (1.b.). This suggests that BS occur more frequently in symptomatically severe patients.
For 39 patients who completed the LBT, a chi-square test between BSA, GSRS, and LBT variables yielded a p< 0.0001 with the proximity matrix table showing that the BSA had a greater overlap with GSRS than the LBT (Table 1).
Discussion: BS analysis using DSP may be a useful objective non-invasive point-of-care metric in monitoring IBS severity. Furthermore, bowel sound analysis correlates with lactulose breath testing, often used on IBS patients. Future work should evaluate clinical utility.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sachin N. Mysore, BA1, Zahf Shaikh, DO2, Shiv Patel, BS3, Neel Godbole, 4, Zamir S. Brelvi, MD, PhD5, Sourav Dutta, MD6. P2339 - Correlation of Point-of-Care, Digital Signal Processed, Bowel Sounds With Lactulose Breath Testing in Patients With Irritable Bowel Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1EndoLogic, Edison, NJ; 2Hackensack University Medical Center, Randolph, NJ; 3Endologic LLC, Parsippany, NJ; 4Brown University, Parsippany, NJ; 5Endologic LLC, Montville, NJ; 6Endologic, Franklin Lakes, NJ
Introduction: Irritable Bowel Syndrome (IBS) is a functional motility disorder characterized by abdominal pain, bloating, and abnormal stool. Our previous study demonstrated that bowel sound analysis (BSA) correlates with symptom severity in patients with IBS. In this study, we develop a model to identify bowel sound events (BSEs) and analyze how bowel sound scores (BS) are associated with IBS symptom severity and Lactulose breath testing (LBT) in an outpatient clinical setting. Digital Signal Processing (DSP) provides a tool to quantify and study BS in motility disorders like IBS.
Methods: This retrospective case-control study includes IBS patients who met Rome IV criteria. Patients completed the Gastrointestinal Symptom Rating Scale (GSRS-IBS) pre-appointment. A score ≥35 was considered an IBS flare-up. BS were recorded from 3 points 4 cm left, right, and below the umbilicus for 15 seconds each with an electronic stethoscope. BSEs were identified using a proprietary algorithm that uses proven DSP methods relating to time and frequency analysis. BSEs were characterized by a BSA score, whose value increases with the number of detected events, and the duration between BSEs. Patients received TrioSmart LBT (Gemelli Biotech) to complete post-appointment.
Results: 127 patients meeting Rome IV criteria were evaluated with the GSRS, yielding 74 patients with active flare-ups (GSRS ≥35) and 53 patients in a symptomatically quiescent state (GSRS < 35). Comparing symptom scores with the BSA scores yielded a scatterplot with an R2 = 0.582 and an ANOVA of regression yielding a p< 0.001 (1.a.). The scatterplot shows a cutoff BS score of 8.5. This yields 72 patients with active flare-ups (BSA ≥8.5) and 55 in a symptomatically quiescent state (BSA < 8.5).
Analyzing the duration between BSEs, patients with GSRS ≥35 had a median duration of 1.07 seconds vs 2.15 seconds for patients < 35. A Pearson’s R test between both sets yields a p< 0.005 (1.b.). This suggests that BS occur more frequently in symptomatically severe patients.
For 39 patients who completed the LBT, a chi-square test between BSA, GSRS, and LBT variables yielded a p< 0.0001 with the proximity matrix table showing that the BSA had a greater overlap with GSRS than the LBT (Table 1).
Discussion: BS analysis using DSP may be a useful objective non-invasive point-of-care metric in monitoring IBS severity. Furthermore, bowel sound analysis correlates with lactulose breath testing, often used on IBS patients. Future work should evaluate clinical utility.
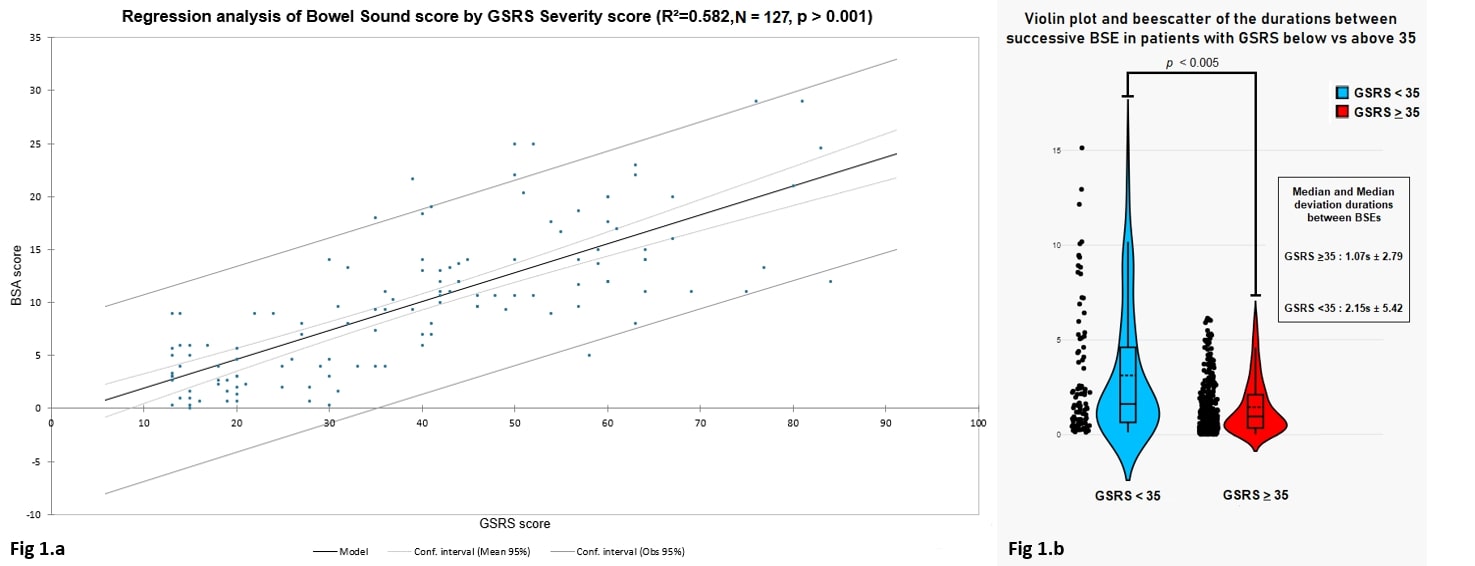
Figure: Figure 1.a: Scatterplot between patient-reported symptom severity (GSRS-IBS) scores and Calculated Bowel Sound Analysis scores.
Figure 1.b: Violin plot and Beescatter showing the recorded durations between BSEs between patients in a symptomatically quiescent state (GSRS<35) and symptomatically severe state (GSRS≥35)
Figure 1.b: Violin plot and Beescatter showing the recorded durations between BSEs between patients in a symptomatically quiescent state (GSRS<35) and symptomatically severe state (GSRS≥35)
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sachin Mysore indicated no relevant financial relationships.
Zahf Shaikh indicated no relevant financial relationships.
Shiv Patel indicated no relevant financial relationships.
Neel Godbole indicated no relevant financial relationships.
Zamir Brelvi indicated no relevant financial relationships.
Sourav Dutta indicated no relevant financial relationships.
Sachin N. Mysore, BA1, Zahf Shaikh, DO2, Shiv Patel, BS3, Neel Godbole, 4, Zamir S. Brelvi, MD, PhD5, Sourav Dutta, MD6. P2339 - Correlation of Point-of-Care, Digital Signal Processed, Bowel Sounds With Lactulose Breath Testing in Patients With Irritable Bowel Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
