Monday Poster Session
Category: Functional Bowel Disease
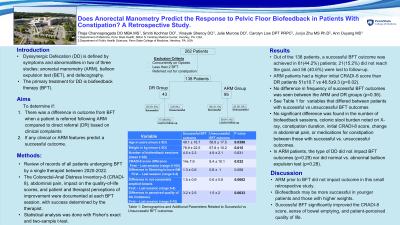
P2340 - Does Anorectal Manometry Predict the Response to Pelvic Floor Biofeedback in Patients With Constipation? A Retrospective Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Theja Channapragada, DO, MBA, MS
Penn State Health Milton S. Hershey Medical Center
Springfield, NJ
Presenting Author(s)
Theja Channapragada, DO, MBA, MS1, Smriti Kochhar, DO2, Vinayak Shenoy, DO2, Julie Murone, DO2, Carolyn Low, 2, Junjia Zhu, MS, PhD3, Ann Ouyang, MD2
1Penn State Health Milton S. Hershey Medical Center, Springfield, NJ; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 3Penn State College of Medicine, Hershey, PA
Introduction: Dyssynergic defecation (DD) is defined by symptoms and abnormalities in 2 of 3 studies: anorectal manometry (ARM), balloon expulsion test, and defecography. The primary treatment for DD is biofeedback therapy (BFT). This study aimed to determine if there was a difference in outcome from BFT when a patient is referred following ARM compared to direct referral (DR) based on clinical complaints and if any clinical or ARM features predict a successful outcome.
Methods: Records of 262 patients who underwent BFT by a single therapist between 2020-2022 were reviewed. Only patients referred for constipation, on no opioids, and with more than 2 BFT sessions were included. This left 138 patients of whom 95 had undergone ARM and BFT (ARM group), and 43 directly referred for BFT without ARM (DR group). The Colorectal-Anal Distress Inventory-8 (CRADI-8), abdominal pain, impact on the quality-of-life scores, and patient and therapist perceptions of improvement were documented at each BFT session, with success determined by the therapist. Between-group comparisons were performed using Fisher’s exact test and 2-sample t-test as appropriate. Data is shown as mean ± SD.
Results: A successful outcome was achieved in 61(44.2%) patients; 21(15.2%) did not reach the goal, and 56 (40.6%) were lost to follow-up. No difference in outcomes was seen between the ARM and DR groups (p=0.36). In ARM patients, the type of DD did not impact BFT outcomes (p=0.29) nor did normal vs. abnormal balloon expulsion test (p=0.28). Those with successful outcomes were younger, had higher initial weight, greater improvements in CRADI-8 score, sense of bowel emptying, patient-perceived quality of life scores, and perception of outcome (Table 1). ARM patients had a higher initial CRADI-8 score than DR patients 51±10.7 vs 46.5±9.3 (p=0.02). No significant difference was found in the number of biofeedback sessions, colonic stool burden noted on X-ray, constipation duration, initial CRADI-8 score, change in abdominal pain, or medications for constipation between those with successful vs. unsuccessful outcomes.
Discussion: In this study, ARM prior to BFT did not impact outcome. Biofeedback may be more successful in younger patients and those with higher weights. Successful BFT significantly improved the CRADI-8 score, sense of bowel emptying, and patient-perceived quality of life. Finding factors that predict a higher success rate is important given relative scarcity of motility centers and pelvic floor biofeedback.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Theja Channapragada, DO, MBA, MS1, Smriti Kochhar, DO2, Vinayak Shenoy, DO2, Julie Murone, DO2, Carolyn Low, 2, Junjia Zhu, MS, PhD3, Ann Ouyang, MD2. P2340 - Does Anorectal Manometry Predict the Response to Pelvic Floor Biofeedback in Patients With Constipation? A Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Springfield, NJ; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 3Penn State College of Medicine, Hershey, PA
Introduction: Dyssynergic defecation (DD) is defined by symptoms and abnormalities in 2 of 3 studies: anorectal manometry (ARM), balloon expulsion test, and defecography. The primary treatment for DD is biofeedback therapy (BFT). This study aimed to determine if there was a difference in outcome from BFT when a patient is referred following ARM compared to direct referral (DR) based on clinical complaints and if any clinical or ARM features predict a successful outcome.
Methods: Records of 262 patients who underwent BFT by a single therapist between 2020-2022 were reviewed. Only patients referred for constipation, on no opioids, and with more than 2 BFT sessions were included. This left 138 patients of whom 95 had undergone ARM and BFT (ARM group), and 43 directly referred for BFT without ARM (DR group). The Colorectal-Anal Distress Inventory-8 (CRADI-8), abdominal pain, impact on the quality-of-life scores, and patient and therapist perceptions of improvement were documented at each BFT session, with success determined by the therapist. Between-group comparisons were performed using Fisher’s exact test and 2-sample t-test as appropriate. Data is shown as mean ± SD.
Results: A successful outcome was achieved in 61(44.2%) patients; 21(15.2%) did not reach the goal, and 56 (40.6%) were lost to follow-up. No difference in outcomes was seen between the ARM and DR groups (p=0.36). In ARM patients, the type of DD did not impact BFT outcomes (p=0.29) nor did normal vs. abnormal balloon expulsion test (p=0.28). Those with successful outcomes were younger, had higher initial weight, greater improvements in CRADI-8 score, sense of bowel emptying, patient-perceived quality of life scores, and perception of outcome (Table 1). ARM patients had a higher initial CRADI-8 score than DR patients 51±10.7 vs 46.5±9.3 (p=0.02). No significant difference was found in the number of biofeedback sessions, colonic stool burden noted on X-ray, constipation duration, initial CRADI-8 score, change in abdominal pain, or medications for constipation between those with successful vs. unsuccessful outcomes.
Discussion: In this study, ARM prior to BFT did not impact outcome. Biofeedback may be more successful in younger patients and those with higher weights. Successful BFT significantly improved the CRADI-8 score, sense of bowel emptying, and patient-perceived quality of life. Finding factors that predict a higher success rate is important given relative scarcity of motility centers and pelvic floor biofeedback.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Theja Channapragada indicated no relevant financial relationships.
Smriti Kochhar indicated no relevant financial relationships.
Vinayak Shenoy indicated no relevant financial relationships.
Julie Murone indicated no relevant financial relationships.
Carolyn Low indicated no relevant financial relationships.
Junjia Zhu indicated no relevant financial relationships.
Ann Ouyang indicated no relevant financial relationships.
Theja Channapragada, DO, MBA, MS1, Smriti Kochhar, DO2, Vinayak Shenoy, DO2, Julie Murone, DO2, Carolyn Low, 2, Junjia Zhu, MS, PhD3, Ann Ouyang, MD2. P2340 - Does Anorectal Manometry Predict the Response to Pelvic Floor Biofeedback in Patients With Constipation? A Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
