Monday Poster Session
Category: Functional Bowel Disease
P2349 - Single-Center Experience with Concomitant Use of Novel and Off-Label Prescriptions for Chronic Constipation
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

MariaLisa Itzoe, DO, MPH
Maimonides Medical Center
Brooklyn, NY
Presenting Author(s)
MariaLisa S. M.. Itzoe, DO, MPH1, Tushar Khanna, MD2, Josh Mukherjee, 2, Nitin Ahuja, MD, MS3
1Maimonides Medical Center, Brooklyn, NY; 2Penn Medicine, Philadelphia, PA; 3University of Pennsylvania, Philadelphia, PA
Introduction: Patients seeking care for constipation in neurogastroenterology and motility (NGM) clinics often have persistent symptoms for which over-the-counter therapies prove ineffective. Many new therapies have been approved recently for chronic idiopathic constipation and irritable bowel syndrome with constipation, though data are limited on their real-world application, including concomitant use of multiple agents and off-label therapies. Via the electronic health record, we aimed to review prescribing patterns within our tertiary-care center among patients with chronic constipation.
Methods: Consecutive patients with 1 of 13 constipation diagnosis codes who were seen by 1 of 5 NGM clinicians were included in this analysis. Charts were reviewed for prescriptions of at least 1 of 8 pharmacotherapies: linaclotide, lubiprostone, plecanatide, prucalopride, tenapanor, tegaserod, pyridostigmine, and colchicine. Data on patient demographics, clinicians, diagnosis codes, and medication initiation and discontinuation were collected and analyzed with descriptive statistics.
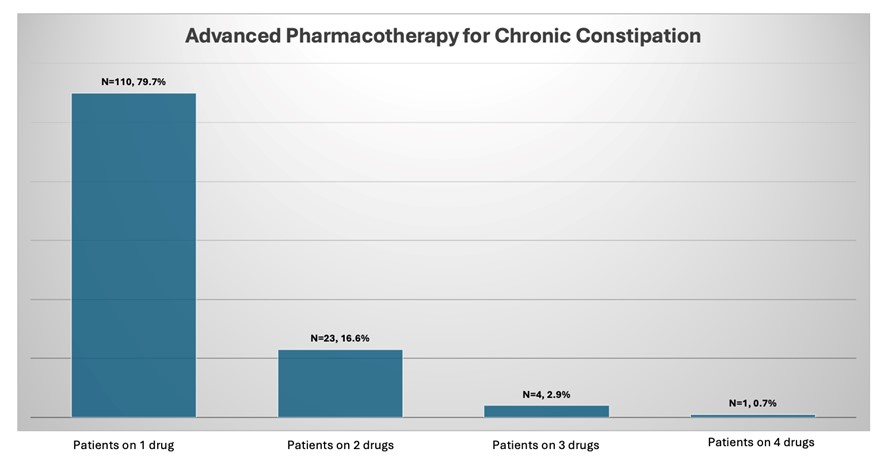
Results: 405 patients were evaluated for chronic constipation, of which 138 (34%) received one or more prescription-based therapies. The most common diagnoses supporting these prescriptions are listed in Table 1. 110 patients (79.7%) were prescribed monotherapy, 23 (16.67%) given dual therapy simultaneously, 4 (2.8%) given three agents simultaneously, and only 1 (0.7%) given four agents simultaneously. The most common monotherapies were linaclotide (49%) and prucalopride (37%). The most common dual therapy regimens were prucalopride + linaclotide (n=14, 61%) followed by prucalopride + lubiprostone (n=3, 13%). Patients on 1-2 concomitant prescriptions had varied distribution of diagnosis codes relative to patients on 3-4 concomitant prescriptions. There were no statistically significant differences in prescribing trends across providers.
Discussion: Real-world prescribing patterns of advanced pharmacotherapies for chronic constipation are varied. While single-agent therapy predominated in this analysis, a clinical strategy of deliberate polypharmacy was observed across providers and diagnoses. Linaclotide and prucalopride were the most common prescriptions utilized either as monotherapy or in combination. Future studies might consider potential reasons both for and against concomitant medication use, including payor considerations and treatment response.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
MariaLisa S. M.. Itzoe, DO, MPH1, Tushar Khanna, MD2, Josh Mukherjee, 2, Nitin Ahuja, MD, MS3. P2349 - Single-Center Experience with Concomitant Use of Novel and Off-Label Prescriptions for Chronic Constipation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Maimonides Medical Center, Brooklyn, NY; 2Penn Medicine, Philadelphia, PA; 3University of Pennsylvania, Philadelphia, PA
Introduction: Patients seeking care for constipation in neurogastroenterology and motility (NGM) clinics often have persistent symptoms for which over-the-counter therapies prove ineffective. Many new therapies have been approved recently for chronic idiopathic constipation and irritable bowel syndrome with constipation, though data are limited on their real-world application, including concomitant use of multiple agents and off-label therapies. Via the electronic health record, we aimed to review prescribing patterns within our tertiary-care center among patients with chronic constipation.
Methods: Consecutive patients with 1 of 13 constipation diagnosis codes who were seen by 1 of 5 NGM clinicians were included in this analysis. Charts were reviewed for prescriptions of at least 1 of 8 pharmacotherapies: linaclotide, lubiprostone, plecanatide, prucalopride, tenapanor, tegaserod, pyridostigmine, and colchicine. Data on patient demographics, clinicians, diagnosis codes, and medication initiation and discontinuation were collected and analyzed with descriptive statistics.
Results: 405 patients were evaluated for chronic constipation, of which 138 (34%) received one or more prescription-based therapies. The most common diagnoses supporting these prescriptions are listed in Table 1. 110 patients (79.7%) were prescribed monotherapy, 23 (16.67%) given dual therapy simultaneously, 4 (2.8%) given three agents simultaneously, and only 1 (0.7%) given four agents simultaneously. The most common monotherapies were linaclotide (49%) and prucalopride (37%). The most common dual therapy regimens were prucalopride + linaclotide (n=14, 61%) followed by prucalopride + lubiprostone (n=3, 13%). Patients on 1-2 concomitant prescriptions had varied distribution of diagnosis codes relative to patients on 3-4 concomitant prescriptions. There were no statistically significant differences in prescribing trends across providers.
Discussion: Real-world prescribing patterns of advanced pharmacotherapies for chronic constipation are varied. While single-agent therapy predominated in this analysis, a clinical strategy of deliberate polypharmacy was observed across providers and diagnoses. Linaclotide and prucalopride were the most common prescriptions utilized either as monotherapy or in combination. Future studies might consider potential reasons both for and against concomitant medication use, including payor considerations and treatment response.
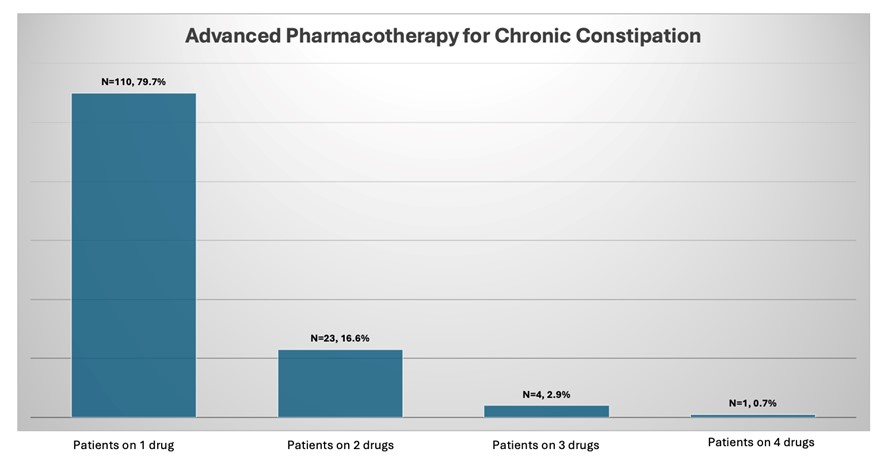
Figure: Figure 1. Distribution of patients with chronic constipation diagnoses prescribed advanced pharmacotherapies
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
MariaLisa Itzoe indicated no relevant financial relationships.
Tushar Khanna indicated no relevant financial relationships.
Josh Mukherjee indicated no relevant financial relationships.
Nitin Ahuja: Ardelyx – Consultant. Eli Lilly – Consultant. Haleon – Consultant. Vanda – Grant/Research Support.
MariaLisa S. M.. Itzoe, DO, MPH1, Tushar Khanna, MD2, Josh Mukherjee, 2, Nitin Ahuja, MD, MS3. P2349 - Single-Center Experience with Concomitant Use of Novel and Off-Label Prescriptions for Chronic Constipation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
