Monday Poster Session
Category: Functional Bowel Disease
P2353 - Anorectal Manometry Biofeedback Therapy for Defecation Disorders: Response Rate and Factors Predicting Improvement
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- DR
Daniel Rim, MD
Lewis Katz School of Medicine at Temple University
Philadelphia, PA
Presenting Author(s)
Daniel Rim, MD1, Henry P. Parkman, MD2
1Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 2Temple University, Philadelphia, PA
Introduction: Anorectal manometry (ARM) biofeedback (BF) is a frequently recommended approach for managing chronic constipation from dyssynergic defecation (DD). There remains a dearth of understanding regarding the distinct patient profiles seeking BF and the identifying features of individuals who might respond favorably to this intervention. This study aims to assess patient responses to ARM BF and characteristics suggesting a favorable response.
Methods: ARM BF was performed using 3 weekly sessions teaching patients to strengthen intrarectal pressure while relaxing the anal sphincter during simulated defecation in patients with constipation. Patients’ characteristics, DD type, and classification of the patient using the London Classification were collected during their diagnostic ARM and first BF session, and their clinical and manometric response to BF was evaluated during their subsequent BF sessions.
Results: Among the 40 patients with defecation disorders undergoing ARM BF, 28 (70%) reported that BF was helpful. 38 (95%) had manometric evidence of DD; type 3 (35%) being the most common. The most common anorectal disorders per London Classification were combined anal hypotension and hypocontractility (37.8%), normal expulsion with abnormal manometric pattern of rectoanal coordination (40.5%), and rectal hypersensitivity (70.3%). With the biofeedback therapy, 21 (55.3%) patients no longer had abnormal manometric patterns. Type 3 and type 4 DD patterns had higher favorable responses (71.4% and 80%, respectively). Normal expulsion with abnormal manometric pattern of rectoanal coordination was found to have the highest favorable response (80%) among disorders of rectoanal coordination. Anal hypertension and rectal hyposensitivity were associated with lower (58.3%) and similar (71.4%) favorable responses compared to the overall response, despite higher rates (70% and 85.7%, respectively) of resolution of DD pattern.
Discussion: Overall, 70% of patients undergoing ARM BF for defecation disorders found biofeedback to be helpful; 55.3% had resolution of manometric evidence of DD. Possible characteristics associated with better response were identified, including the presence of type 3 and type 4 DD manometric patterns. These findings will help inform patients of the improvement they may have with biofeedback treatment based on their symptoms and baseline manometric findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Daniel Rim, MD1, Henry P. Parkman, MD2. P2353 - Anorectal Manometry Biofeedback Therapy for Defecation Disorders: Response Rate and Factors Predicting Improvement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 2Temple University, Philadelphia, PA
Introduction: Anorectal manometry (ARM) biofeedback (BF) is a frequently recommended approach for managing chronic constipation from dyssynergic defecation (DD). There remains a dearth of understanding regarding the distinct patient profiles seeking BF and the identifying features of individuals who might respond favorably to this intervention. This study aims to assess patient responses to ARM BF and characteristics suggesting a favorable response.
Methods: ARM BF was performed using 3 weekly sessions teaching patients to strengthen intrarectal pressure while relaxing the anal sphincter during simulated defecation in patients with constipation. Patients’ characteristics, DD type, and classification of the patient using the London Classification were collected during their diagnostic ARM and first BF session, and their clinical and manometric response to BF was evaluated during their subsequent BF sessions.
Results: Among the 40 patients with defecation disorders undergoing ARM BF, 28 (70%) reported that BF was helpful. 38 (95%) had manometric evidence of DD; type 3 (35%) being the most common. The most common anorectal disorders per London Classification were combined anal hypotension and hypocontractility (37.8%), normal expulsion with abnormal manometric pattern of rectoanal coordination (40.5%), and rectal hypersensitivity (70.3%). With the biofeedback therapy, 21 (55.3%) patients no longer had abnormal manometric patterns. Type 3 and type 4 DD patterns had higher favorable responses (71.4% and 80%, respectively). Normal expulsion with abnormal manometric pattern of rectoanal coordination was found to have the highest favorable response (80%) among disorders of rectoanal coordination. Anal hypertension and rectal hyposensitivity were associated with lower (58.3%) and similar (71.4%) favorable responses compared to the overall response, despite higher rates (70% and 85.7%, respectively) of resolution of DD pattern.
Discussion: Overall, 70% of patients undergoing ARM BF for defecation disorders found biofeedback to be helpful; 55.3% had resolution of manometric evidence of DD. Possible characteristics associated with better response were identified, including the presence of type 3 and type 4 DD manometric patterns. These findings will help inform patients of the improvement they may have with biofeedback treatment based on their symptoms and baseline manometric findings.
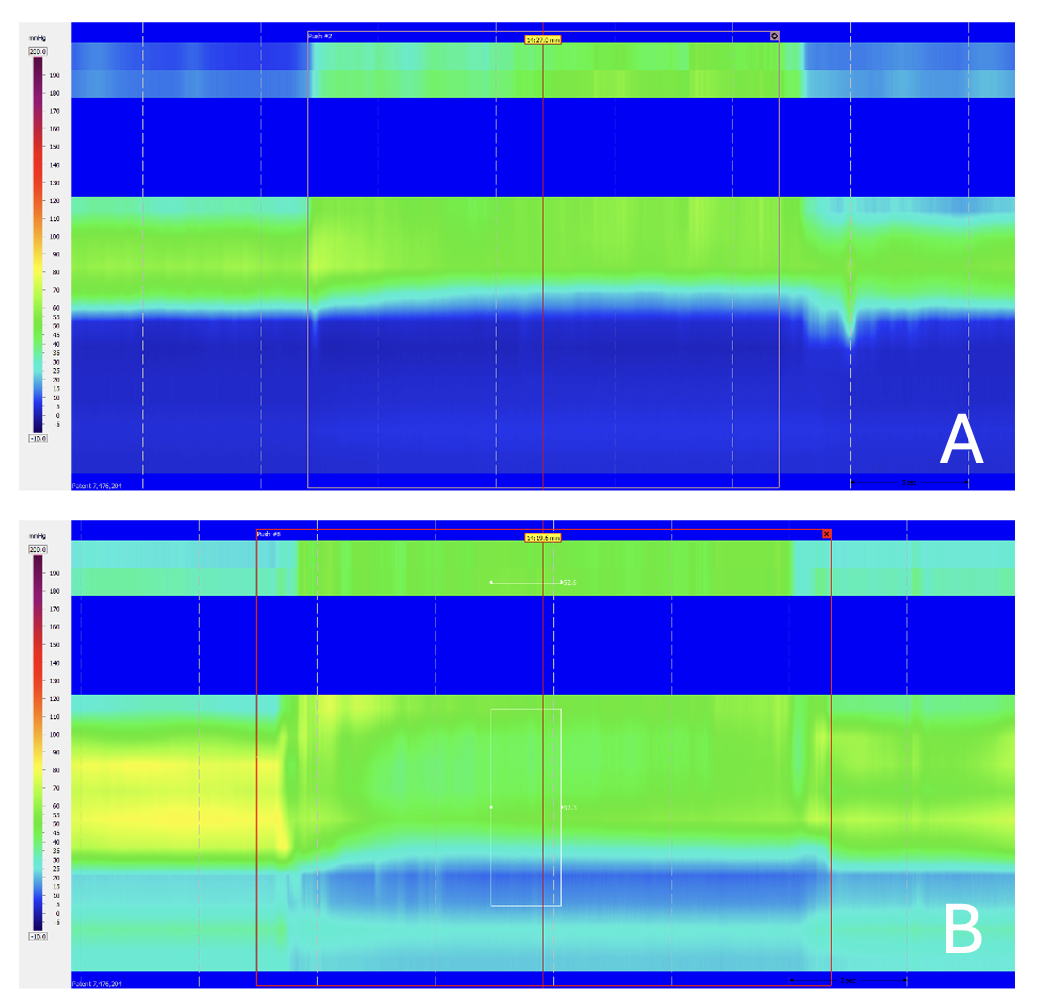
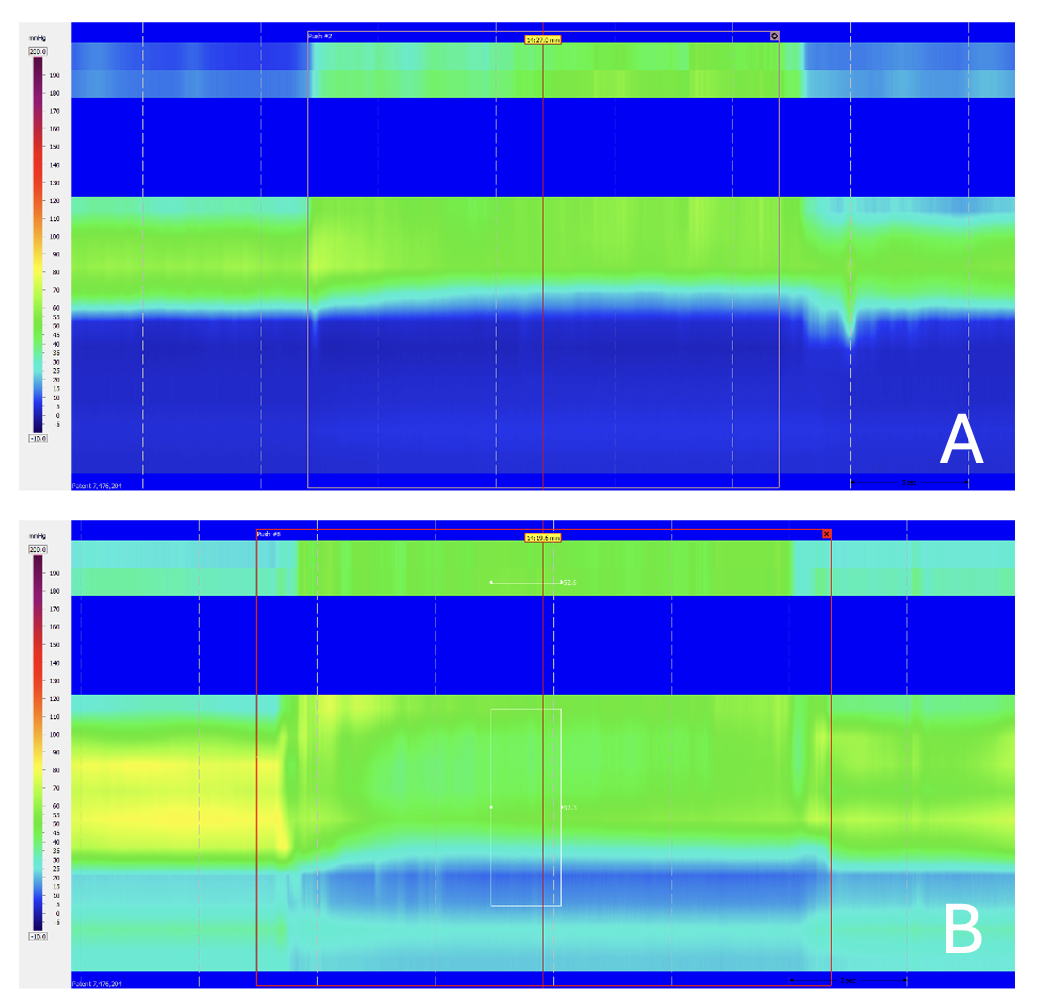
Figure: Image A shows a dyssynergic defecation pattern before biofeedback therapy. Image B shows a normal manometric pattern after biofeedback therapy.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Daniel Rim indicated no relevant financial relationships.
Henry Parkman: Alimetry – Grant/Research Support. Cin Dom Pharma – Consultant. Evoke Pharma – Consultant. Medtronic Enterra – Consultant. Takeda Pharma – Consultant.
Daniel Rim, MD1, Henry P. Parkman, MD2. P2353 - Anorectal Manometry Biofeedback Therapy for Defecation Disorders: Response Rate and Factors Predicting Improvement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
