Monday Poster Session
Category: Functional Bowel Disease
P2354 - Amitriptyline Efficacy in Irritable Bowel Syndrome: A Comprehensive Meta-Analysis of Randomized Controlled Trials
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Vikash Kumar, MD
Creighton University School of Medicine
Brooklyn, NY
Presenting Author(s)
Madho Mal, MBBS1, Rahul Kumar, MD2, Herby Jeanty, MD3, Fnu Vikash, MD, M.Med4, Nayanika Chowdary. Tummala, MBBS5, Nisma Faridi, MBBS6, Shahrob Khan, MBBS7, Diksha Kajal, MD,8, Gautam Maddineni, MD9, Arnold N. Forlemu, MD, MPH10, Vikash Kumar, MD11, Aalam Sohal, MD12, Ali Wakil, MD3, Vijay Bhaskar Reddy Gayam, MD13
1Queen's University School of Medicine, Karachi, Sindh, Pakistan; 2Jacobi/ North Central Bronx Hospital Bronx, Bronx, NY; 3Brooklyn Hospital Center, Brooklyn, NY; 4Albert Einstein College of Medicine, New York, NY; 5Gitam Institute of Medical Sciences and Research, Secunderaabad, Telangana, India; 6Army Medical College, Islamabad, Islamabad, Pakistan; 7Federal Government Polyclinic, Islamabad, Islamabad, Pakistan; 8Florida State University College of Medicine, Cape Coral, FL; 9Florida State University, Cape Coral, FL; 10Brooklyn Hospital Center, Athens, GA; 11Creighton University School of Medicine, Brooklyn, NY; 12Creighton University School of Medicine, Seattle, WA; 13University of Texas Southwestern, Dallas, TX
Introduction: Irritable bowel syndrome (IBS) presents a considerable challenge in clinical management, necessitating effective therapeutic interventions to alleviate symptoms and improve quality of life. Amitriptyline, a tricyclic antidepressant, has shown promise as a potential treatment for IBS due to its effects on pain modulation and gastrointestinal motility. This study aims to comprehensively evaluate the effectiveness of amitriptyline as a therapeutic intervention for IBS through a meta-analysis of randomized controlled trials.
Methods: A systematic search was conducted across reputable databases including PubMed, Scopus, Web of Science, and the Cochrane Central Register of Controlled Trials, covering the years 1966 to 2023. Double-blind, placebo-controlled randomized control trials investigating the efficacy of amitriptyline in IBS management were identified and included in the analysis. Studies were included if they involved adult participants diagnosed with IBS who had an indication for amitriptyline treatment. Data extraction and quality assessment were performed in accordance with established guidelines for systematic reviews and meta-analyses.
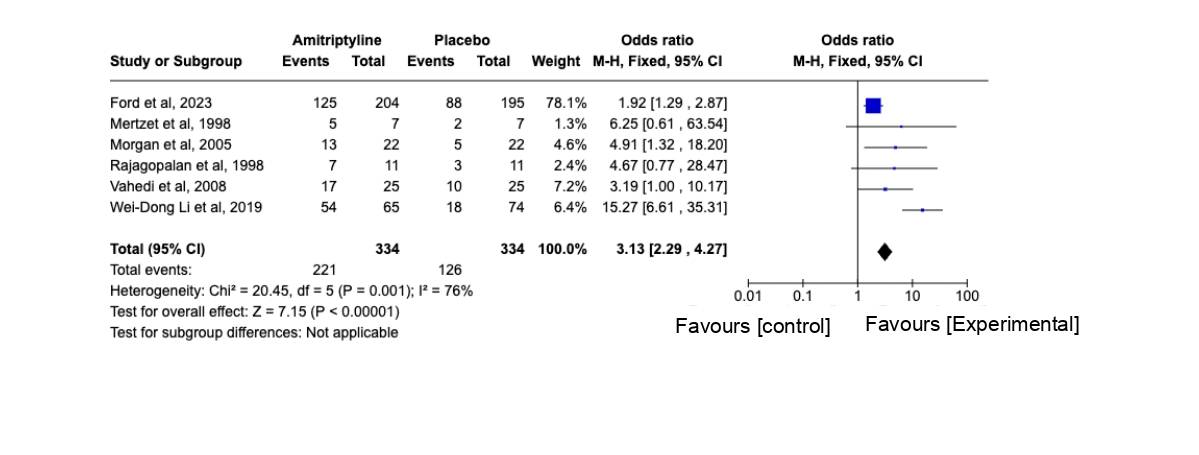
Results: The meta-analysis included 6 randomized, placebo-controlled trials with 668 participants. Amitriptyline significantly improved IBS symptoms, with a pooled odds ratio (OR) of 3.13 (95% CI: 2.29 to 4.27, p< 0.00001). Despite moderate heterogeneity (I² = 76%, p=0.001), the fixed-effect model showed consistent benefit across studies. Notably, Wei-Dong Li et al. (2019) reported the highest OR of 15.27 (95% CI: 6.61 to 35.31). Smaller sample sizes in some studies, like Rajagopalan et al (1998), may explain the lack of statistical significance.
Discussion: This meta-analysis confirms that amitriptyline significantly improves IBS symptoms compared to placebo, with an odds ratio of 3.13. The findings support amitriptyline as an effective therapeutic option for IBS, especially for patients unresponsive to conventional treatments. Future research should focus on optimal dosing, patient subgroups, and long-term safety. Amitriptyline's inclusion in treatment plans could enhance quality of life for those with IBS.
Disclosures:
Madho Mal, MBBS1, Rahul Kumar, MD2, Herby Jeanty, MD3, Fnu Vikash, MD, M.Med4, Nayanika Chowdary. Tummala, MBBS5, Nisma Faridi, MBBS6, Shahrob Khan, MBBS7, Diksha Kajal, MD,8, Gautam Maddineni, MD9, Arnold N. Forlemu, MD, MPH10, Vikash Kumar, MD11, Aalam Sohal, MD12, Ali Wakil, MD3, Vijay Bhaskar Reddy Gayam, MD13. P2354 - Amitriptyline Efficacy in Irritable Bowel Syndrome: A Comprehensive Meta-Analysis of Randomized Controlled Trials, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Queen's University School of Medicine, Karachi, Sindh, Pakistan; 2Jacobi/ North Central Bronx Hospital Bronx, Bronx, NY; 3Brooklyn Hospital Center, Brooklyn, NY; 4Albert Einstein College of Medicine, New York, NY; 5Gitam Institute of Medical Sciences and Research, Secunderaabad, Telangana, India; 6Army Medical College, Islamabad, Islamabad, Pakistan; 7Federal Government Polyclinic, Islamabad, Islamabad, Pakistan; 8Florida State University College of Medicine, Cape Coral, FL; 9Florida State University, Cape Coral, FL; 10Brooklyn Hospital Center, Athens, GA; 11Creighton University School of Medicine, Brooklyn, NY; 12Creighton University School of Medicine, Seattle, WA; 13University of Texas Southwestern, Dallas, TX
Introduction: Irritable bowel syndrome (IBS) presents a considerable challenge in clinical management, necessitating effective therapeutic interventions to alleviate symptoms and improve quality of life. Amitriptyline, a tricyclic antidepressant, has shown promise as a potential treatment for IBS due to its effects on pain modulation and gastrointestinal motility. This study aims to comprehensively evaluate the effectiveness of amitriptyline as a therapeutic intervention for IBS through a meta-analysis of randomized controlled trials.
Methods: A systematic search was conducted across reputable databases including PubMed, Scopus, Web of Science, and the Cochrane Central Register of Controlled Trials, covering the years 1966 to 2023. Double-blind, placebo-controlled randomized control trials investigating the efficacy of amitriptyline in IBS management were identified and included in the analysis. Studies were included if they involved adult participants diagnosed with IBS who had an indication for amitriptyline treatment. Data extraction and quality assessment were performed in accordance with established guidelines for systematic reviews and meta-analyses.
Results: The meta-analysis included 6 randomized, placebo-controlled trials with 668 participants. Amitriptyline significantly improved IBS symptoms, with a pooled odds ratio (OR) of 3.13 (95% CI: 2.29 to 4.27, p< 0.00001). Despite moderate heterogeneity (I² = 76%, p=0.001), the fixed-effect model showed consistent benefit across studies. Notably, Wei-Dong Li et al. (2019) reported the highest OR of 15.27 (95% CI: 6.61 to 35.31). Smaller sample sizes in some studies, like Rajagopalan et al (1998), may explain the lack of statistical significance.
Discussion: This meta-analysis confirms that amitriptyline significantly improves IBS symptoms compared to placebo, with an odds ratio of 3.13. The findings support amitriptyline as an effective therapeutic option for IBS, especially for patients unresponsive to conventional treatments. Future research should focus on optimal dosing, patient subgroups, and long-term safety. Amitriptyline's inclusion in treatment plans could enhance quality of life for those with IBS.
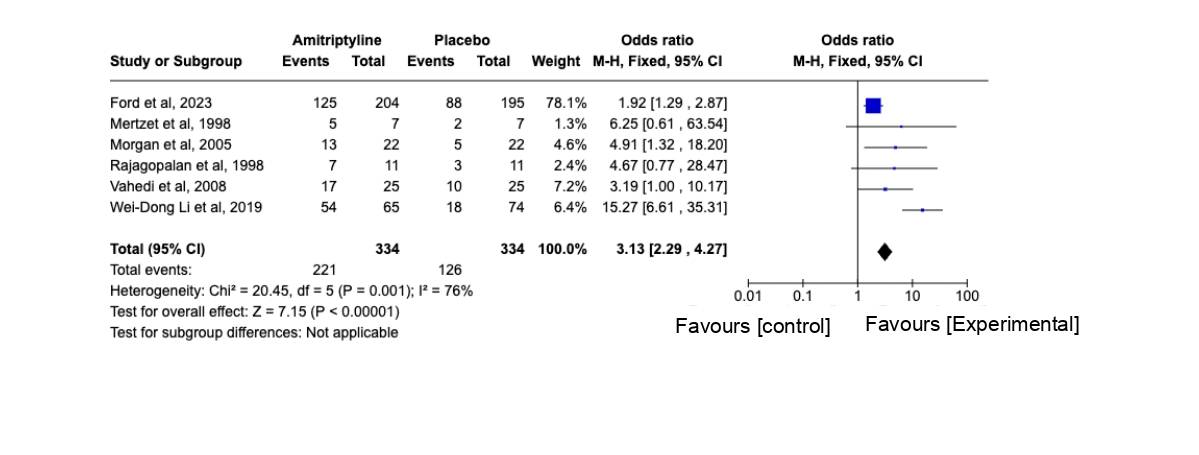
Figure:
Disclosures:
Madho Mal indicated no relevant financial relationships.
Rahul Kumar indicated no relevant financial relationships.
Herby Jeanty indicated no relevant financial relationships.
Fnu Vikash indicated no relevant financial relationships.
Nayanika Tummala indicated no relevant financial relationships.
Nisma Faridi indicated no relevant financial relationships.
Shahrob Khan indicated no relevant financial relationships.
Diksha Kajal indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Arnold Forlemu indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Ali Wakil indicated no relevant financial relationships.
Vijay Bhaskar Reddy Gayam indicated no relevant financial relationships.
Madho Mal, MBBS1, Rahul Kumar, MD2, Herby Jeanty, MD3, Fnu Vikash, MD, M.Med4, Nayanika Chowdary. Tummala, MBBS5, Nisma Faridi, MBBS6, Shahrob Khan, MBBS7, Diksha Kajal, MD,8, Gautam Maddineni, MD9, Arnold N. Forlemu, MD, MPH10, Vikash Kumar, MD11, Aalam Sohal, MD12, Ali Wakil, MD3, Vijay Bhaskar Reddy Gayam, MD13. P2354 - Amitriptyline Efficacy in Irritable Bowel Syndrome: A Comprehensive Meta-Analysis of Randomized Controlled Trials, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
