Monday Poster Session
Category: Functional Bowel Disease
P2364 - Irritable Bowel Syndrome or Acute Intermittent Porphyria - The Clinical Conundrum in Healthy Young Individuals
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Selena Zhou, MD
David Geffen School of Medicine at UCLA
Los Angeles, CA
Presenting Author(s)
Award: Presidential Poster Award
Selena Zhou, MD1, Robert Tamai, MD1, Guy A. Weiss, MD2
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2UCLA, Los Angeles, CA
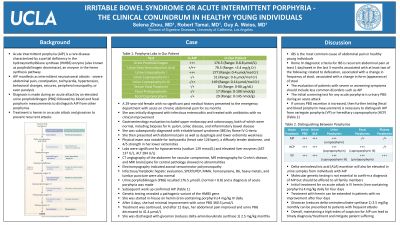
Introduction: Acute intermittent porphyria (AIP) is a rare disease caused by a deficiency in the hydroxymethylbilane synthase (HMBS) enzyme. AIP manifests as intermittent neurovisceral attacks, most commonly severe abdominal pain. We present a case of AIP misdiagnosed for several months as irritable bowel syndrome - constipation (IBS-C) requiring extended treatment.
Case Description/Methods: A 29-year-old female with no significant past medical history presented to the emergency department with acute on chronic abdominal pain for six months. She was initially diagnosed with infectious enterocolitis and treated with antibiotics with no clinical improvement. Gastroenterology evaluation included upper endoscopy and colonoscopy, both of which were normal, including biopsies for H. pylori, celiac disease, and inflammatory bowel disease. She was subsequently diagnosed with IBS-C by Rome IV Criteria.
She then presented with abdominal pain as well as dysphagia and lower extremity weakness. Physical exam was notable for tachycardia (heart rate 126 bpm), a diffusely tender abdomen, and 4/5 strength in her lower extremities. Labs were significant for hyponatremia (sodium 129 mmol/L) and elevated liver enzymes (AST 137 U/L, ALT 284 U/L).
CT angiography of the abdomen for vascular compromise, MR enterography for Crohn’s disease, and MRI brain/spine for central pathology showed no abnormalities. Electromyography indicated axonal sensorimotor polyneuropathy. Infectious/metabolic hepatic evaluation, SPEP/UPEP, MMA, homocysteine, B6, heavy metals, and lumbar puncture were also normal. Urine porphobilinogen (PBG) resulted 176.5 µmol/L (normal < 8.8) and a diagnosis of acute porphyria was made. Subsequent work up confirmed AIP (Table 1). Genetic testing revealed a pathogenic variant of the HMBS gene.
She was started in-house on hemin (iron-containing porphyrin) 4 mg/kg IV daily. After 4 days, she had minimal improvement with urine PBG 360.5 µmol/L. Treatment was continued, and after 12 days, her abdominal pain improved and urine PBG decreased to 41.4 µmol/L. She was discharged with givosiran (reduces delta-aminolevulinate synthase 1).
Discussion: IBS is the most common cause of abdominal pain in healthy young individuals, but the evaluation of patients with severe or worsening symptoms should include less common disorders such as AIP. Maintaining a high index of suspicion can lead to timely diagnosis/treatment and mitigate patient suffering. Treatment with hemin can be extended in patients with no improvement after four days.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Selena Zhou, MD1, Robert Tamai, MD1, Guy A. Weiss, MD2. P2364 - Irritable Bowel Syndrome or Acute Intermittent Porphyria - The Clinical Conundrum in Healthy Young Individuals, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Selena Zhou, MD1, Robert Tamai, MD1, Guy A. Weiss, MD2
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2UCLA, Los Angeles, CA
Introduction: Acute intermittent porphyria (AIP) is a rare disease caused by a deficiency in the hydroxymethylbilane synthase (HMBS) enzyme. AIP manifests as intermittent neurovisceral attacks, most commonly severe abdominal pain. We present a case of AIP misdiagnosed for several months as irritable bowel syndrome - constipation (IBS-C) requiring extended treatment.
Case Description/Methods: A 29-year-old female with no significant past medical history presented to the emergency department with acute on chronic abdominal pain for six months. She was initially diagnosed with infectious enterocolitis and treated with antibiotics with no clinical improvement. Gastroenterology evaluation included upper endoscopy and colonoscopy, both of which were normal, including biopsies for H. pylori, celiac disease, and inflammatory bowel disease. She was subsequently diagnosed with IBS-C by Rome IV Criteria.
She then presented with abdominal pain as well as dysphagia and lower extremity weakness. Physical exam was notable for tachycardia (heart rate 126 bpm), a diffusely tender abdomen, and 4/5 strength in her lower extremities. Labs were significant for hyponatremia (sodium 129 mmol/L) and elevated liver enzymes (AST 137 U/L, ALT 284 U/L).
CT angiography of the abdomen for vascular compromise, MR enterography for Crohn’s disease, and MRI brain/spine for central pathology showed no abnormalities. Electromyography indicated axonal sensorimotor polyneuropathy. Infectious/metabolic hepatic evaluation, SPEP/UPEP, MMA, homocysteine, B6, heavy metals, and lumbar puncture were also normal. Urine porphobilinogen (PBG) resulted 176.5 µmol/L (normal < 8.8) and a diagnosis of acute porphyria was made. Subsequent work up confirmed AIP (Table 1). Genetic testing revealed a pathogenic variant of the HMBS gene.
She was started in-house on hemin (iron-containing porphyrin) 4 mg/kg IV daily. After 4 days, she had minimal improvement with urine PBG 360.5 µmol/L. Treatment was continued, and after 12 days, her abdominal pain improved and urine PBG decreased to 41.4 µmol/L. She was discharged with givosiran (reduces delta-aminolevulinate synthase 1).
Discussion: IBS is the most common cause of abdominal pain in healthy young individuals, but the evaluation of patients with severe or worsening symptoms should include less common disorders such as AIP. Maintaining a high index of suspicion can lead to timely diagnosis/treatment and mitigate patient suffering. Treatment with hemin can be extended in patients with no improvement after four days.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Selena Zhou indicated no relevant financial relationships.
Robert Tamai indicated no relevant financial relationships.
Guy Weiss: Everlywell – Consultant. Guidepoint consulting – Consultant. Regeneron – Consultant.
Selena Zhou, MD1, Robert Tamai, MD1, Guy A. Weiss, MD2. P2364 - Irritable Bowel Syndrome or Acute Intermittent Porphyria - The Clinical Conundrum in Healthy Young Individuals, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

