Monday Poster Session
Category: Functional Bowel Disease
P2366 - Chronic Tirzepatide Use Mimics Histology Findings of Celiac Disease: A Case Report
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MC
Muntha Chaudhari, MBBS
Shalamar Hospital Pakistan
Lahore, Punjab, Pakistan
Presenting Author(s)
Ahtshamullah Chaudhry, MD1, Jawad Noor, MD1, Gabriel Buluku, MD1, Bharat Malhotra, MD2, Muntha Chaudhari, MBBS3, Makau lee, MD, PhD4
1Franciscan Missionaries of Our Lady Health System, Jackson, MS; 2fmolhs, Jackson, MS; 3Shalamar Hospital Pakistan, Lahore, Punjab, Pakistan; 4University of Mississippi Medical Center, Jackson, MS
Introduction: Tirzepatide, a dual GLP-1 and GIP receptor agonist, is used for type 2 diabetes and weight loss, often causing gastrointestinal side effects like nausea, vomiting, and diarrhea. In rare cases, its use can mimic celiac disease histologically. Here we present a case where tirzepatide induced GI side effects were caused by histological features mimicking celiac disease.
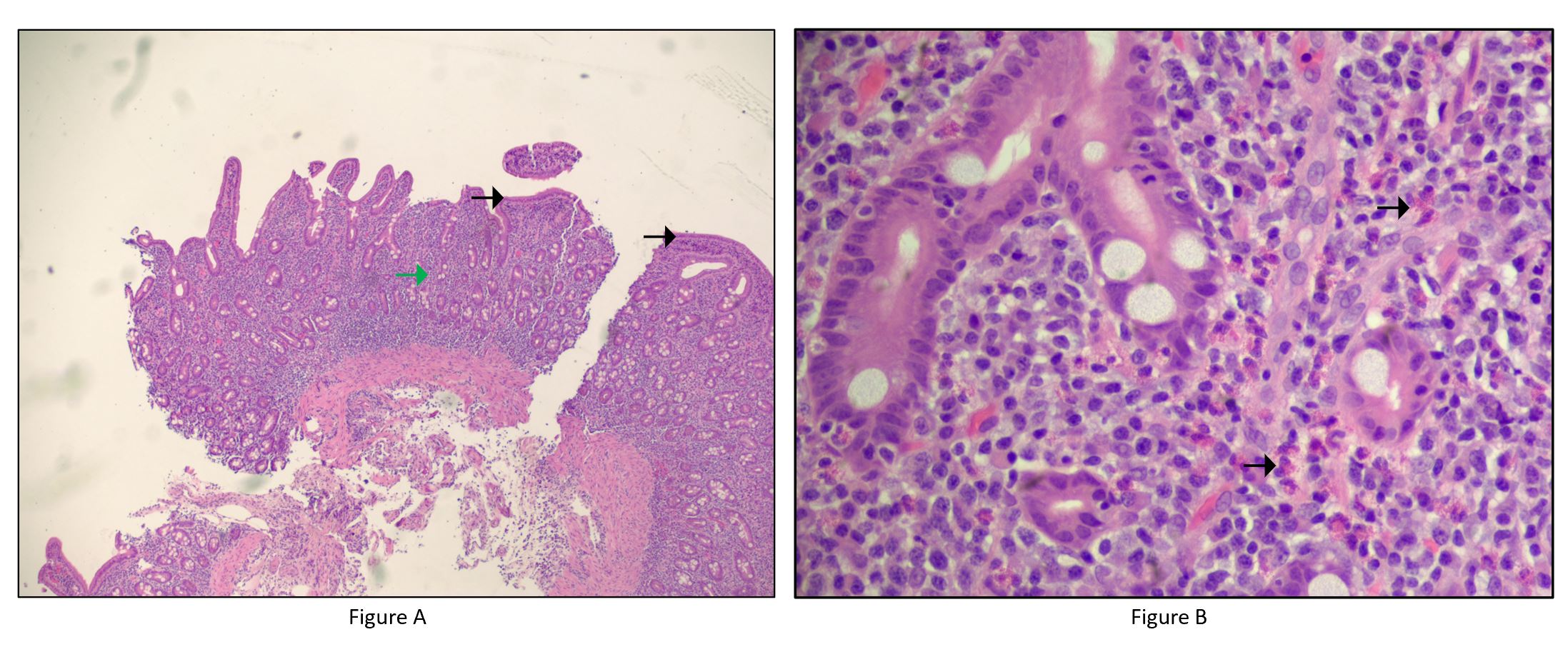
Case Description/Methods: A 58-year-old man with a past medical history of Hypertension and Type 2 diabetes mellitus presented with profuse watery diarrhea. His symptoms started after taking Tirzepatide 10 mg, with 15 to 20 episodes each day. For the past 18 months, he has been taking tirzepatide (10 mg weekly). Computed tomography of the abdomen and pelvis showed no acute findings. Labs showed potassium of 4.2 mmol/l, white blood count of 12.4 ul, and his lipase was 75 u/l. His. We discontinued tirzepatide, administered normal saline, and ruled out enteric pathogens with negative stool studies. Esophagogastroduodenoscopy revealed diffusely blunted villi in the mucosa of the first and second parts of the duodenum, with cold biopsies taken. Sigmoidoscopy showed diffuse granularity, and cold biopsies were also performed. His symptoms began to improve. Antinuclear antibody testing was negative, reducing suspicion of an autoimmune process, so further autoimmune workup was deemed unnecessary given his improving condition. Colon biopsy showed no evidence of collagenous or microscopic colitis. However, duodenal biopsy showed duodenitis with significant villous blunting, dense chronic inflammation in the lamina propria (Figure 1A), and eosinophilia (Figure 1B). His symptoms improved with supportive treatment, tirzepatide was discontinued, and he was discharged home.
Discussion: We present a case of a young man admitted for profuse diarrhea. Workups for infectious and autoimmune causes were inconclusive. Esophagogastroduodenoscopy and duodenal biopsy showed duodenitis with considerable villous blunting, dense chronic inflammation, and eosinophilia, resembling Celiac disease. Symptoms improved after stopping Tirzepatide, suggesting it as the likely cause. The mechanism by which Tirzepatide induces such histological features is unclear but may involve gut inflammation and barrier impairment leading to bacterial translocation and gastrointestinal symptoms. Dietary triggers like gluten and fermentable oligosaccharides, disaccharides, monosaccharides, and polyols might exacerbate these effects. Further studies are needed to explore these mechanisms and optimize management.
Disclosures:
Ahtshamullah Chaudhry, MD1, Jawad Noor, MD1, Gabriel Buluku, MD1, Bharat Malhotra, MD2, Muntha Chaudhari, MBBS3, Makau lee, MD, PhD4. P2366 - Chronic Tirzepatide Use Mimics Histology Findings of Celiac Disease: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Franciscan Missionaries of Our Lady Health System, Jackson, MS; 2fmolhs, Jackson, MS; 3Shalamar Hospital Pakistan, Lahore, Punjab, Pakistan; 4University of Mississippi Medical Center, Jackson, MS
Introduction: Tirzepatide, a dual GLP-1 and GIP receptor agonist, is used for type 2 diabetes and weight loss, often causing gastrointestinal side effects like nausea, vomiting, and diarrhea. In rare cases, its use can mimic celiac disease histologically. Here we present a case where tirzepatide induced GI side effects were caused by histological features mimicking celiac disease.
Case Description/Methods: A 58-year-old man with a past medical history of Hypertension and Type 2 diabetes mellitus presented with profuse watery diarrhea. His symptoms started after taking Tirzepatide 10 mg, with 15 to 20 episodes each day. For the past 18 months, he has been taking tirzepatide (10 mg weekly). Computed tomography of the abdomen and pelvis showed no acute findings. Labs showed potassium of 4.2 mmol/l, white blood count of 12.4 ul, and his lipase was 75 u/l. His. We discontinued tirzepatide, administered normal saline, and ruled out enteric pathogens with negative stool studies. Esophagogastroduodenoscopy revealed diffusely blunted villi in the mucosa of the first and second parts of the duodenum, with cold biopsies taken. Sigmoidoscopy showed diffuse granularity, and cold biopsies were also performed. His symptoms began to improve. Antinuclear antibody testing was negative, reducing suspicion of an autoimmune process, so further autoimmune workup was deemed unnecessary given his improving condition. Colon biopsy showed no evidence of collagenous or microscopic colitis. However, duodenal biopsy showed duodenitis with significant villous blunting, dense chronic inflammation in the lamina propria (Figure 1A), and eosinophilia (Figure 1B). His symptoms improved with supportive treatment, tirzepatide was discontinued, and he was discharged home.
Discussion: We present a case of a young man admitted for profuse diarrhea. Workups for infectious and autoimmune causes were inconclusive. Esophagogastroduodenoscopy and duodenal biopsy showed duodenitis with considerable villous blunting, dense chronic inflammation, and eosinophilia, resembling Celiac disease. Symptoms improved after stopping Tirzepatide, suggesting it as the likely cause. The mechanism by which Tirzepatide induces such histological features is unclear but may involve gut inflammation and barrier impairment leading to bacterial translocation and gastrointestinal symptoms. Dietary triggers like gluten and fermentable oligosaccharides, disaccharides, monosaccharides, and polyols might exacerbate these effects. Further studies are needed to explore these mechanisms and optimize management.
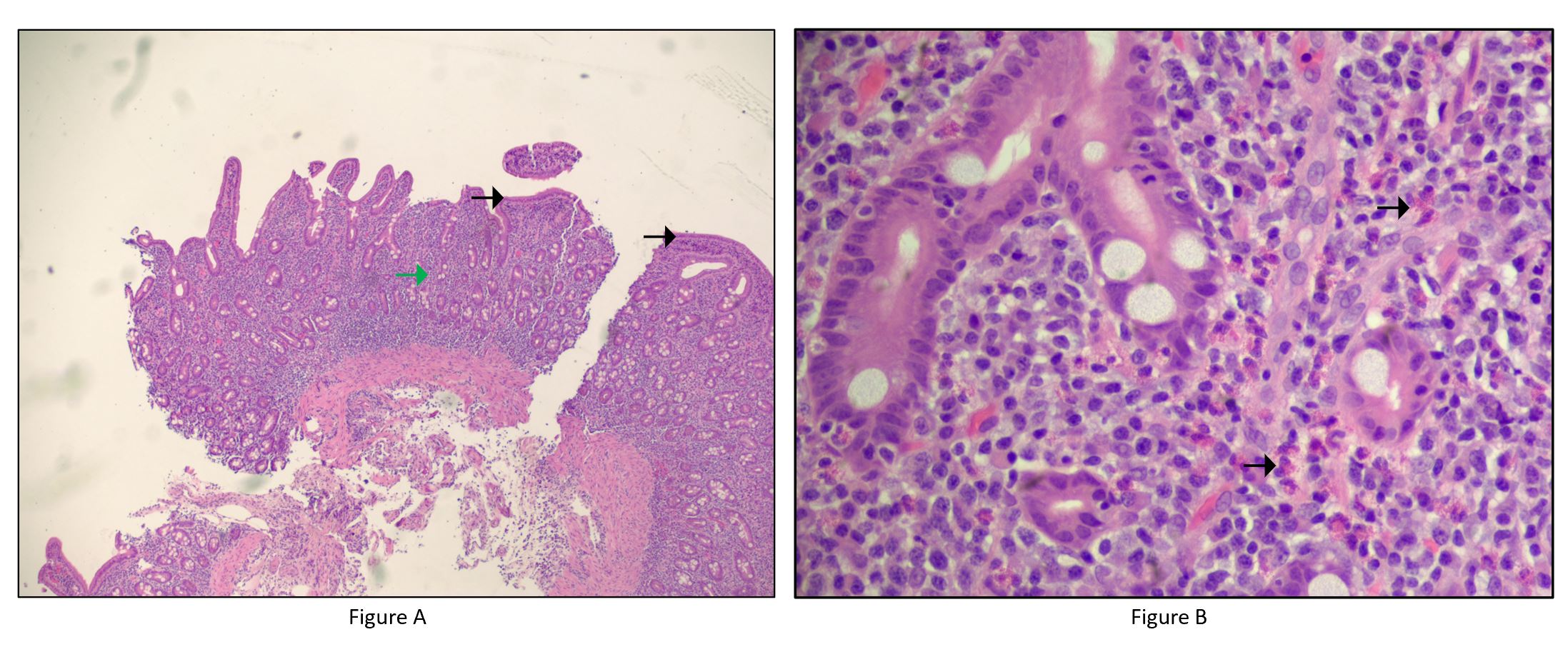
Figure: Figure A: Duodenal mucosa shows villous blunting (black arrows) and dense chronic inflammation in the lamina propria (green arrow)
Figure B: Duodenal mucosa has increased eosinophils (black arrows)
Figure B: Duodenal mucosa has increased eosinophils (black arrows)
Disclosures:
Ahtshamullah Chaudhry indicated no relevant financial relationships.
Jawad Noor indicated no relevant financial relationships.
Gabriel Buluku indicated no relevant financial relationships.
Bharat Malhotra indicated no relevant financial relationships.
Muntha Chaudhari indicated no relevant financial relationships.
Makau lee indicated no relevant financial relationships.
Ahtshamullah Chaudhry, MD1, Jawad Noor, MD1, Gabriel Buluku, MD1, Bharat Malhotra, MD2, Muntha Chaudhari, MBBS3, Makau lee, MD, PhD4. P2366 - Chronic Tirzepatide Use Mimics Histology Findings of Celiac Disease: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
