Monday Poster Session
Category: General Endoscopy
P2400 - Impact of Dementia on Esophagogastroduodenoscopy (EGD) Outcomes: A Head-to-Head Comparison
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Faris Shweikeh, MD
Cleveland Clinic Akron General
Akron, OH
Presenting Author(s)
Faris Shweikeh, MD1, Colin Fricker, BA2, Raneem Khedraki, PhD3, Amandeep Singh, MD1, Matthew Hoscheit, MD4, Anthony J. Lembo, MD5
1Cleveland Clinic Akron General, Akron, OH; 2Northeast Ohio Medical University, Rootstown, OH; 3Cleveland Clinic, Cleveland, OH; 4Cleveland Clinic Foundation, Cleveland, OH; 5Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
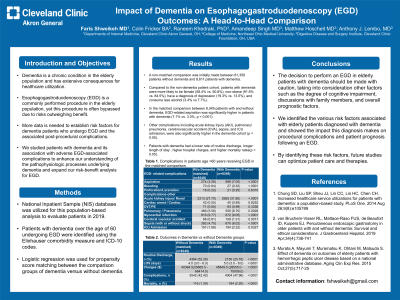
Introduction: Dementia is a chronic condition in the elderly population and has extensive consequences for healthcare utilization. Esophagogastroduodenoscopy (EGD) is a commonly performed procedure in the elderly population, yet this procedure is often bypassed due to risks outweighing benefit. More data is needed to establish risk factors for dementia patients who undergo EGD and the associated post-procedural complications. We studied patients with dementia and its association with adverse EGD-associated complications to enhance our understanding of the pathophysiologic processes underlying dementia and expand our risk-benefit analysis for EGD.
Methods: National Inpatient Sample (NIS) database was utilized for this population-based analysis to evaluate patients in 2019. Patients with dementia over the age of 60 undergoing EGD were identified using the Elixhauser comorbidity measure and ICD-10 codes. Logistic regression was used for propensity score matching between the comparison groups of dementia versus without dementia.
Results: A non-matched comparison was initially made between 81,359 patients without dementia and 8,611 patients with dementia. Compared to the non-dementia patient cohort, patients with dementia were more likely to be female (58.4% vs. 50.8%), non-obese (91.6% vs. 84.5%), have a diagnosis of depression (19.3% vs. 13.5%), and consume less alcohol (3.4% vs 7.7%). In the matched comparison between 8,349 patients with and without dementia, EGD-related aspiration was significantly higher in patients with dementia (7.1% vs. 3.3%, p < 0.001). Other complications including acute kidney injury (AKI), pulmonary/pneumonia, cerebrovascular accident (CVA), sepsis, and ICU admission, were also significantly higher in the dementia cohort (p < 0.05). Patients with dementia had a lower rate of routine discharge, longer length of stay , higher hospital charges , and higher mortality rates(p < 0.05).
Discussion: The decision to perform an EGD in elderly patients with dementia should be made with caution, taking into consideration other factors such as the degree of cognitive impairment, discussions with family members, and overall prognostic factors. We identified the various risk factors associated with elderly patients diagnosed with dementia and showed the impact this diagnosis makes on procedural complications and patient prognosis following an EGD. By identifying these risk factors, future studies can optimize patient care and therapies.
Disclosures:
Faris Shweikeh, MD1, Colin Fricker, BA2, Raneem Khedraki, PhD3, Amandeep Singh, MD1, Matthew Hoscheit, MD4, Anthony J. Lembo, MD5. P2400 - Impact of Dementia on Esophagogastroduodenoscopy (EGD) Outcomes: A Head-to-Head Comparison, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Akron General, Akron, OH; 2Northeast Ohio Medical University, Rootstown, OH; 3Cleveland Clinic, Cleveland, OH; 4Cleveland Clinic Foundation, Cleveland, OH; 5Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
Introduction: Dementia is a chronic condition in the elderly population and has extensive consequences for healthcare utilization. Esophagogastroduodenoscopy (EGD) is a commonly performed procedure in the elderly population, yet this procedure is often bypassed due to risks outweighing benefit. More data is needed to establish risk factors for dementia patients who undergo EGD and the associated post-procedural complications. We studied patients with dementia and its association with adverse EGD-associated complications to enhance our understanding of the pathophysiologic processes underlying dementia and expand our risk-benefit analysis for EGD.
Methods: National Inpatient Sample (NIS) database was utilized for this population-based analysis to evaluate patients in 2019. Patients with dementia over the age of 60 undergoing EGD were identified using the Elixhauser comorbidity measure and ICD-10 codes. Logistic regression was used for propensity score matching between the comparison groups of dementia versus without dementia.
Results: A non-matched comparison was initially made between 81,359 patients without dementia and 8,611 patients with dementia. Compared to the non-dementia patient cohort, patients with dementia were more likely to be female (58.4% vs. 50.8%), non-obese (91.6% vs. 84.5%), have a diagnosis of depression (19.3% vs. 13.5%), and consume less alcohol (3.4% vs 7.7%). In the matched comparison between 8,349 patients with and without dementia, EGD-related aspiration was significantly higher in patients with dementia (7.1% vs. 3.3%, p < 0.001). Other complications including acute kidney injury (AKI), pulmonary/pneumonia, cerebrovascular accident (CVA), sepsis, and ICU admission, were also significantly higher in the dementia cohort (p < 0.05). Patients with dementia had a lower rate of routine discharge, longer length of stay , higher hospital charges , and higher mortality rates(p < 0.05).
Discussion: The decision to perform an EGD in elderly patients with dementia should be made with caution, taking into consideration other factors such as the degree of cognitive impairment, discussions with family members, and overall prognostic factors. We identified the various risk factors associated with elderly patients diagnosed with dementia and showed the impact this diagnosis makes on procedural complications and patient prognosis following an EGD. By identifying these risk factors, future studies can optimize patient care and therapies.
Disclosures:
Faris Shweikeh indicated no relevant financial relationships.
Colin Fricker indicated no relevant financial relationships.
Raneem Khedraki indicated no relevant financial relationships.
Amandeep Singh indicated no relevant financial relationships.
Matthew Hoscheit indicated no relevant financial relationships.
Anthony Lembo: Allurion – Stock Options. Bristol Myers Squibb – Stock Options. Johnson & Johnson – Stock Options. Vibrant Advisory Board – Advisory Committee/Board Member.
Faris Shweikeh, MD1, Colin Fricker, BA2, Raneem Khedraki, PhD3, Amandeep Singh, MD1, Matthew Hoscheit, MD4, Anthony J. Lembo, MD5. P2400 - Impact of Dementia on Esophagogastroduodenoscopy (EGD) Outcomes: A Head-to-Head Comparison, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
