Monday Poster Session
Category: General Endoscopy
P2405 - Adverse Events With Glucagon-Like Peptide-1 Receptor Agonists During Upper Endoscopy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Sahib Singh, MD
Sinai Hospital
Baltimore, MD
Presenting Author(s)
Sahib Singh, MD1, Ayushi Shah, MD2, Yash R. Shah, MD3, Babu Mohan, MD4, Vishnu Charan Suresh Kumar, MD5, Ganesh Aswath, MD5, Rakesh Vinayek, MD1, Dushyant S. Dahiya, MD6, Sumant Inamdar, MD7, Douglas Adler, MD8, Hassam Ali, MD9, Neil R Sharma, MD, FACG10, Sudhir Dutta, MD1
1Sinai Hospital, Baltimore, MD; 2SUNY Upstate Medical University, Omaha, NE; 3Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 4Orlando Gastroenterology PA, Orlando, FL; 5SUNY Upstate Medical University, Syracuse, NY; 6The University of Kansas School of Medicine, Kansas City, KS; 7University of Arkansas for Medical Sciences, Little Rock, AR; 8Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO; 9ECU Health Medical Center, Greenville, NC; 10IOSE. Peak Gastroenterology & Gastrocare Partners., Colorado Springs, CO
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1RAs) are commonly used for weight loss and in patients with diabetes mellitus (DM). They are known to cause delayed gastric emptying, however the effect on clinical outcomes during upper endoscopy remains unclear, with studies reporting conflicting results. We conducted a meta-analysis to reconcile the data.
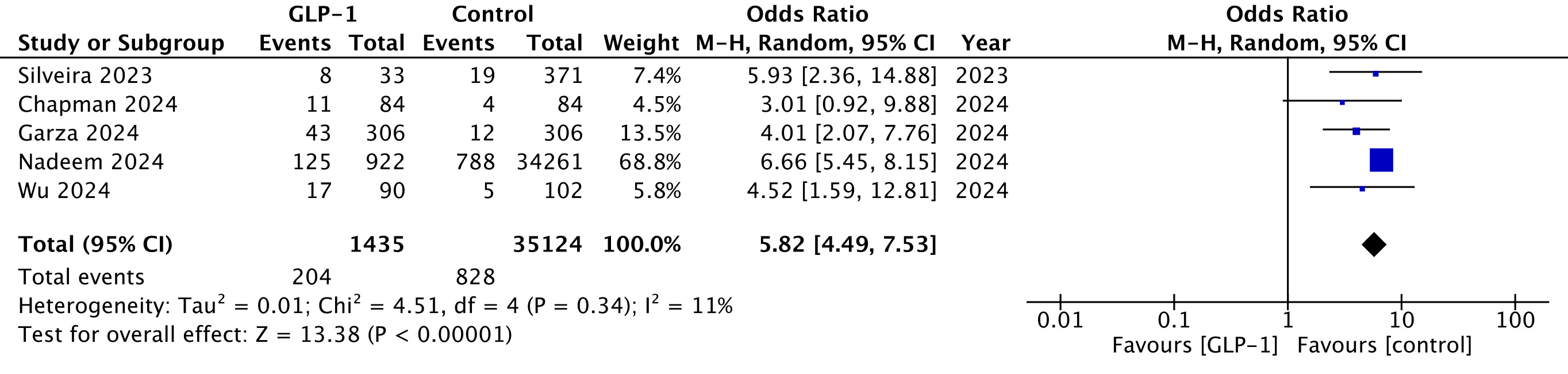
Methods: Online databases were searched for studies evaluating GLP-1RAs vs control group (no GLP-1RAs) in patients undergoing upper endoscopy. The outcomes of interest were rates of retained gastric contents, aspiration, aspiration pneumonia, and aborted endoscopies. Pooled odds ratios (ORs) and 95% confidence intervals (CIs) were estimated using a random-effects model. The I² statistic was used to depict inter-study heterogeneity.
Results: Seven observational studies with patients undergoing a total of 80,045 upper endoscopic procedures (GLP-1 group n=19,926, control group n=60,119) were included. The mean age was 56 years, 43% were men and 63% had DM. As compared to the control group, patients on GLP-1RAs had higher incidence of retained gastric contents (OR 5.82, 95% CI 4.49 - 7.53, p < 0.00001, I² = 11%) (Figure 1). The two groups had similar odds of having aspiration events (OR 3.77, 95% CI 0.42 - 33.75, p = 0.24, I² = 68%) and aspiration pneumonia (OR 1.21, 95% CI 0.67 - 2.17, p = 0.53, I² = 54%). GLP-1RA users had a higher rate of aborted endoscopies (OR 5.23, 95% CI 3.01 - 9.08, p < 0.00001, I² = 0%).
Discussion: Patients on GLP-1RAs have a higher chance of visible retained gastric contents on upper endoscopies and an increased rate of early termination of such endoscopies, when compared with patients not on GLP-1RAs. The risk of developing aspiration or aspiration pneumonia was comparable in the two groups. Further prospective studies would be needed to corroborate these findings.
Disclosures:
Sahib Singh, MD1, Ayushi Shah, MD2, Yash R. Shah, MD3, Babu Mohan, MD4, Vishnu Charan Suresh Kumar, MD5, Ganesh Aswath, MD5, Rakesh Vinayek, MD1, Dushyant S. Dahiya, MD6, Sumant Inamdar, MD7, Douglas Adler, MD8, Hassam Ali, MD9, Neil R Sharma, MD, FACG10, Sudhir Dutta, MD1. P2405 - Adverse Events With Glucagon-Like Peptide-1 Receptor Agonists During Upper Endoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Sinai Hospital, Baltimore, MD; 2SUNY Upstate Medical University, Omaha, NE; 3Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 4Orlando Gastroenterology PA, Orlando, FL; 5SUNY Upstate Medical University, Syracuse, NY; 6The University of Kansas School of Medicine, Kansas City, KS; 7University of Arkansas for Medical Sciences, Little Rock, AR; 8Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO; 9ECU Health Medical Center, Greenville, NC; 10IOSE. Peak Gastroenterology & Gastrocare Partners., Colorado Springs, CO
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1RAs) are commonly used for weight loss and in patients with diabetes mellitus (DM). They are known to cause delayed gastric emptying, however the effect on clinical outcomes during upper endoscopy remains unclear, with studies reporting conflicting results. We conducted a meta-analysis to reconcile the data.
Methods: Online databases were searched for studies evaluating GLP-1RAs vs control group (no GLP-1RAs) in patients undergoing upper endoscopy. The outcomes of interest were rates of retained gastric contents, aspiration, aspiration pneumonia, and aborted endoscopies. Pooled odds ratios (ORs) and 95% confidence intervals (CIs) were estimated using a random-effects model. The I² statistic was used to depict inter-study heterogeneity.
Results: Seven observational studies with patients undergoing a total of 80,045 upper endoscopic procedures (GLP-1 group n=19,926, control group n=60,119) were included. The mean age was 56 years, 43% were men and 63% had DM. As compared to the control group, patients on GLP-1RAs had higher incidence of retained gastric contents (OR 5.82, 95% CI 4.49 - 7.53, p < 0.00001, I² = 11%) (Figure 1). The two groups had similar odds of having aspiration events (OR 3.77, 95% CI 0.42 - 33.75, p = 0.24, I² = 68%) and aspiration pneumonia (OR 1.21, 95% CI 0.67 - 2.17, p = 0.53, I² = 54%). GLP-1RA users had a higher rate of aborted endoscopies (OR 5.23, 95% CI 3.01 - 9.08, p < 0.00001, I² = 0%).
Discussion: Patients on GLP-1RAs have a higher chance of visible retained gastric contents on upper endoscopies and an increased rate of early termination of such endoscopies, when compared with patients not on GLP-1RAs. The risk of developing aspiration or aspiration pneumonia was comparable in the two groups. Further prospective studies would be needed to corroborate these findings.
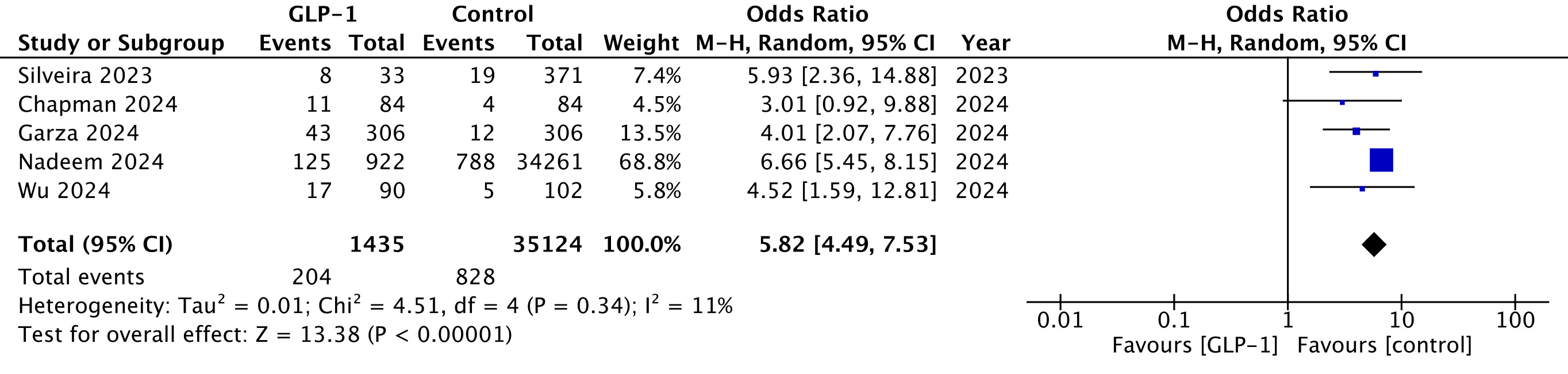
Figure: Retained gastric contents
Disclosures:
Sahib Singh indicated no relevant financial relationships.
Ayushi Shah indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Vishnu Charan Suresh Kumar indicated no relevant financial relationships.
Ganesh Aswath indicated no relevant financial relationships.
Rakesh Vinayek indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Sumant Inamdar indicated no relevant financial relationships.
Douglas Adler: Boston Scientific and Micro Tech. – Consultant.
Hassam Ali indicated no relevant financial relationships.
Neil R Sharma: Boston Scientific – Consultant. Medtronic – Consultant. Olympus – Consultant. Steris – Consultant.
Sudhir Dutta indicated no relevant financial relationships.
Sahib Singh, MD1, Ayushi Shah, MD2, Yash R. Shah, MD3, Babu Mohan, MD4, Vishnu Charan Suresh Kumar, MD5, Ganesh Aswath, MD5, Rakesh Vinayek, MD1, Dushyant S. Dahiya, MD6, Sumant Inamdar, MD7, Douglas Adler, MD8, Hassam Ali, MD9, Neil R Sharma, MD, FACG10, Sudhir Dutta, MD1. P2405 - Adverse Events With Glucagon-Like Peptide-1 Receptor Agonists During Upper Endoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

