Monday Poster Session
Category: General Endoscopy
P2406 - Rare but Real: Abdominal Wall Abscess as a Complication of Percutaneous Endoscopic Gastrostomy Tube Placement in a High-Risk Patient
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MS
Mohammed Rifat Shaik, MBBS
University of Maryland Medical Center Midtown Campus
Baltimore, MD
Presenting Author(s)
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS2, Zainab Mujahid, MD3, Tufan Cinar, MD1, Akshay Duddu, MD4, Aleksan Khachatryan, 5, Joel Manuel Alejandro, MD, MBA1
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2SSM Health/Saint Louis University School of Medicine, St. Louis, MO; 3University of Maryland Capital Region Health, Lorton, VA; 4Greater Baltimore Medical Center, Towson, MD; 5University of Maryland Medical Center, Midtown Campus, Baltimore, MD
Introduction: Percutaneous endoscopic gastrostomy (PEG) has increasingly supplanted surgical gastrostomy as the preferred procedure for providing long-term nutrition to patients with swallowing disorders. While local infectious complications can occur in 5% of cases in non-malignant patients, an abdominal wall abscess is extremely rare. Here, we report a case of an abdominal wall abscess developing within a month of PEG tube placement.
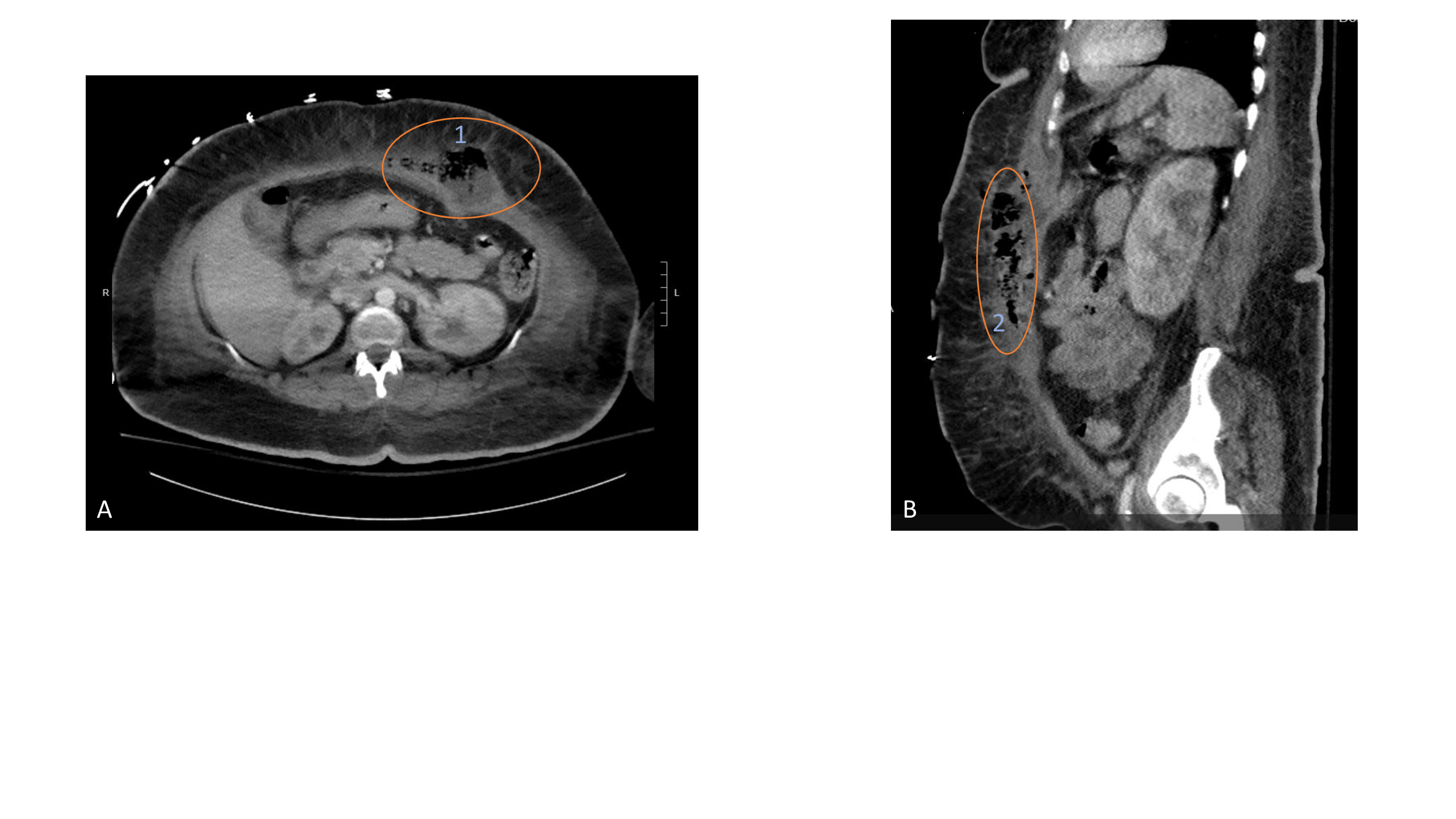
Case Description/Methods: A 53-year-old female with a medical history of multiple strokes, coronary artery disease, pulmonary embolism, right internal jugular thrombosis on anticoagulation, and ventilator dependence s/p tracheostomy was brought in from a nursing home due to lethargy. She had recently undergone PEG tube placement for oropharyngeal dysphagia a month prior. On examination, she was febrile (39.4°C), tachycardic, and tachypneic. Work-up revealed a white blood cell count of 17.1 × 109/L with left shift, platelet count of 470 × 109/L, and erythrocyte sedimentation rate (ESR) of 140 mm/h. Chemistry is remarkable for lactate of 3.8 mmol/L and C-reactive protein (CRP) of 274 mg/L. Chest X-ray and urinalysis were negative for infection. However, a computed tomography (CT) scan of the abdomen showed a dislodged PEG tube with subcutaneous gas and fluid collection concerning for an abdominal wall abscess (Figure). The patient was started on broad-spectrum antibiotics and underwent open placement of a gastrostomy tube and debridement of the abdominal wall abscess. She completed a five-day course of piperacillin-tazobactam therapy. Blood cultures returned negative. Subsequently, she was managed with daily dressing changes and an abdominal binder to protect the gastrostomy tube and wound.
Discussion: Risk factors for infection after PEG tube placement include underlying malignancy, tube size, institutional factors, previous radiation exposure, and cirrhosis. These infections are most common in the first three months. In a prospective study of 1,041 patients receiving a PEG tube, 11.1% experienced local, cutaneous, and peristomal infections. Similarly, another prospective study of 453 patients found that 11% developed peristomal infections and 10% had peristomal leakage. Neither study reported cases of abdominal wall abscesses. However, in a separate prospective study involving 136 patients, one case of an abdominal abscess was documented. Although abdominal abscesses remain a rare complication, treatment involves debridement, tube replacement, and antibiotic therapy.
Disclosures:
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS2, Zainab Mujahid, MD3, Tufan Cinar, MD1, Akshay Duddu, MD4, Aleksan Khachatryan, 5, Joel Manuel Alejandro, MD, MBA1. P2406 - Rare but Real: Abdominal Wall Abscess as a Complication of Percutaneous Endoscopic Gastrostomy Tube Placement in a High-Risk Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2SSM Health/Saint Louis University School of Medicine, St. Louis, MO; 3University of Maryland Capital Region Health, Lorton, VA; 4Greater Baltimore Medical Center, Towson, MD; 5University of Maryland Medical Center, Midtown Campus, Baltimore, MD
Introduction: Percutaneous endoscopic gastrostomy (PEG) has increasingly supplanted surgical gastrostomy as the preferred procedure for providing long-term nutrition to patients with swallowing disorders. While local infectious complications can occur in 5% of cases in non-malignant patients, an abdominal wall abscess is extremely rare. Here, we report a case of an abdominal wall abscess developing within a month of PEG tube placement.
Case Description/Methods: A 53-year-old female with a medical history of multiple strokes, coronary artery disease, pulmonary embolism, right internal jugular thrombosis on anticoagulation, and ventilator dependence s/p tracheostomy was brought in from a nursing home due to lethargy. She had recently undergone PEG tube placement for oropharyngeal dysphagia a month prior. On examination, she was febrile (39.4°C), tachycardic, and tachypneic. Work-up revealed a white blood cell count of 17.1 × 109/L with left shift, platelet count of 470 × 109/L, and erythrocyte sedimentation rate (ESR) of 140 mm/h. Chemistry is remarkable for lactate of 3.8 mmol/L and C-reactive protein (CRP) of 274 mg/L. Chest X-ray and urinalysis were negative for infection. However, a computed tomography (CT) scan of the abdomen showed a dislodged PEG tube with subcutaneous gas and fluid collection concerning for an abdominal wall abscess (Figure). The patient was started on broad-spectrum antibiotics and underwent open placement of a gastrostomy tube and debridement of the abdominal wall abscess. She completed a five-day course of piperacillin-tazobactam therapy. Blood cultures returned negative. Subsequently, she was managed with daily dressing changes and an abdominal binder to protect the gastrostomy tube and wound.
Discussion: Risk factors for infection after PEG tube placement include underlying malignancy, tube size, institutional factors, previous radiation exposure, and cirrhosis. These infections are most common in the first three months. In a prospective study of 1,041 patients receiving a PEG tube, 11.1% experienced local, cutaneous, and peristomal infections. Similarly, another prospective study of 453 patients found that 11% developed peristomal infections and 10% had peristomal leakage. Neither study reported cases of abdominal wall abscesses. However, in a separate prospective study involving 136 patients, one case of an abdominal abscess was documented. Although abdominal abscesses remain a rare complication, treatment involves debridement, tube replacement, and antibiotic therapy.
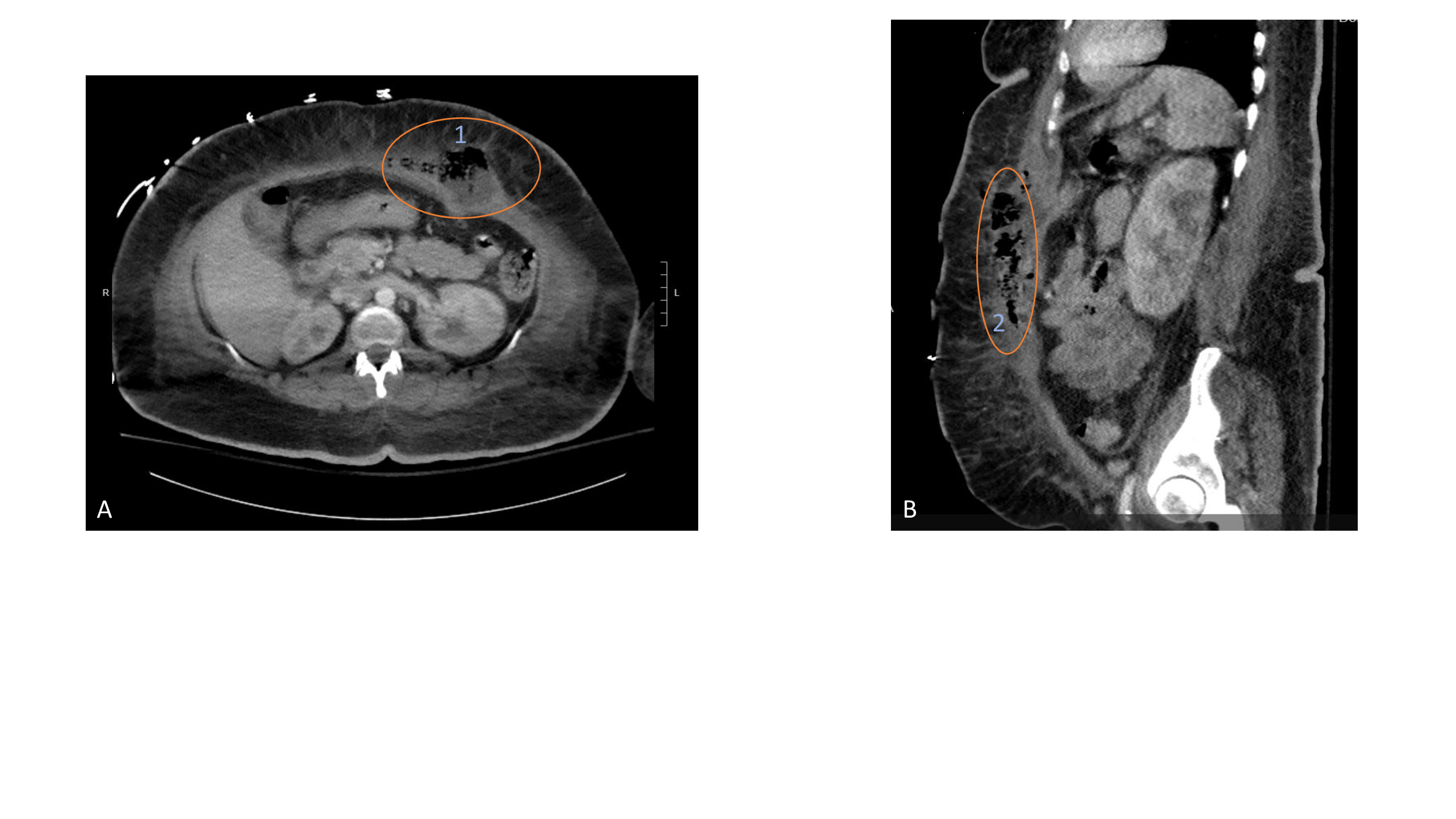
Figure: A and B are cross-sectional and sagittal view images of CT abdomen showing an abdominal wall abscess measuring 8.0 x 4.7 cm in cross-section (1) and 12.9 cm longitudinally (2). Note the adjacent inflammatory stranding of the subcutaneous fat and overlying dermal thickening.
Disclosures:
Mohammed Rifat Shaik indicated no relevant financial relationships.
Nishat Anjum Shaik indicated no relevant financial relationships.
Zainab Mujahid indicated no relevant financial relationships.
Tufan Cinar indicated no relevant financial relationships.
Akshay Duddu indicated no relevant financial relationships.
Aleksan Khachatryan indicated no relevant financial relationships.
Joel Manuel Alejandro indicated no relevant financial relationships.
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS2, Zainab Mujahid, MD3, Tufan Cinar, MD1, Akshay Duddu, MD4, Aleksan Khachatryan, 5, Joel Manuel Alejandro, MD, MBA1. P2406 - Rare but Real: Abdominal Wall Abscess as a Complication of Percutaneous Endoscopic Gastrostomy Tube Placement in a High-Risk Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
