Monday Poster Session
Category: General Endoscopy
P2429 - Eosinophilic Gastroenterocolitis in an Elderly Patient Presented With Persistent Diarrhea
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Zeinab Bakhshizarrinabadi, MD
St. Luke's Hospital
St. Louis, MO
Presenting Author(s)
Zeinab Bakhshizarrinabadi, MD, Elie chahla, MD
St. Luke's Hospital, St. Louis, MO
Introduction: Eosinophilic gastrointestinal disease commonly occurs in the esophagus. Involvement of the stomach and small intestine is less common, and eosinophilic colitis is an exceptionally rare condition, with few cases reported.
Case Description/Methods: A 77-year-old female patient with a history of gastroesophageal reflux disease, hypertension, Raynaud's phenomena, vitamin D deficiency, and asthma presented with persistent diarrhea. Her symptoms began eight days prior to admission, occurring 3-6 times a day. The patient initially self-administered bismuth subsalicylate and loperamide, with no relief.
The patient denied any recent travel and had no recent exposure to animals, sick individuals, swimming water, or pets. She was afebrile with a normal heart rate and blood pressure of 116/63 mmHg. Her physical examination revealed normal findings.
Upon admission, her lab results were notable for a white blood cell count of 26,100/μL, a neutrophil count of 14,600/μL, an eosinophil count of 7,300/μL, hemoglobin of 14 g/dL, and platelets of 277,000/μL. Her metabolic panel showed elevated alkaline phosphatase at 237 U/L, bicarbonate at 20 mmol/L, and normal electrolytes. Lactate was normal, and C-reactive protein was 3.8 mg/L. A fecal occult blood test was positive, and enteric stool pathogen testing was negative.
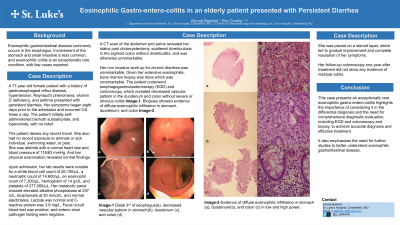
A CT scan of the abdomen and pelvis revealed her status post cholecystectomy, scattered diverticulosis in the sigmoid colon without diverticulitis, and was otherwise unremarkable. Extensive rheumatologic, autoimmune, and oncologic evaluations were unremarkable. The patient underwent esophagogastroduodenoscopy (EGD) and colonoscopy, which revealed a decreased vascular pattern in the duodenum and colon without severe or obvious colitis. Biopsies showed evidence of diffuse eosinophilic infiltration in the stomach, duodenum, and colon.
She was placed on a steroid taper, which led to gradual improvement and complete resolution of her symptoms. Her follow-up colonoscopy one year after treatment did not show any evidence of residual colitis.
Discussion: This case of exceptionally rare eosinophilic gastroenterocolitis highlights the importance of considering it in the differential diagnosis and the need for comprehensive diagnostic evaluation, including EGD, colonoscopy, and biopsy, to achieve accurate diagnosis and effective treatment. It also emphasizes the need for further studies to better understand eosinophilic gastrointestinal disease.
Disclosures:
Zeinab Bakhshizarrinabadi, MD, Elie chahla, MD. P2429 - Eosinophilic Gastroenterocolitis in an Elderly Patient Presented With Persistent Diarrhea, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
St. Luke's Hospital, St. Louis, MO
Introduction: Eosinophilic gastrointestinal disease commonly occurs in the esophagus. Involvement of the stomach and small intestine is less common, and eosinophilic colitis is an exceptionally rare condition, with few cases reported.
Case Description/Methods: A 77-year-old female patient with a history of gastroesophageal reflux disease, hypertension, Raynaud's phenomena, vitamin D deficiency, and asthma presented with persistent diarrhea. Her symptoms began eight days prior to admission, occurring 3-6 times a day. The patient initially self-administered bismuth subsalicylate and loperamide, with no relief.
The patient denied any recent travel and had no recent exposure to animals, sick individuals, swimming water, or pets. She was afebrile with a normal heart rate and blood pressure of 116/63 mmHg. Her physical examination revealed normal findings.
Upon admission, her lab results were notable for a white blood cell count of 26,100/μL, a neutrophil count of 14,600/μL, an eosinophil count of 7,300/μL, hemoglobin of 14 g/dL, and platelets of 277,000/μL. Her metabolic panel showed elevated alkaline phosphatase at 237 U/L, bicarbonate at 20 mmol/L, and normal electrolytes. Lactate was normal, and C-reactive protein was 3.8 mg/L. A fecal occult blood test was positive, and enteric stool pathogen testing was negative.
A CT scan of the abdomen and pelvis revealed her status post cholecystectomy, scattered diverticulosis in the sigmoid colon without diverticulitis, and was otherwise unremarkable. Extensive rheumatologic, autoimmune, and oncologic evaluations were unremarkable. The patient underwent esophagogastroduodenoscopy (EGD) and colonoscopy, which revealed a decreased vascular pattern in the duodenum and colon without severe or obvious colitis. Biopsies showed evidence of diffuse eosinophilic infiltration in the stomach, duodenum, and colon.
She was placed on a steroid taper, which led to gradual improvement and complete resolution of her symptoms. Her follow-up colonoscopy one year after treatment did not show any evidence of residual colitis.
Discussion: This case of exceptionally rare eosinophilic gastroenterocolitis highlights the importance of considering it in the differential diagnosis and the need for comprehensive diagnostic evaluation, including EGD, colonoscopy, and biopsy, to achieve accurate diagnosis and effective treatment. It also emphasizes the need for further studies to better understand eosinophilic gastrointestinal disease.
Disclosures:
Zeinab Bakhshizarrinabadi indicated no relevant financial relationships.
Elie chahla indicated no relevant financial relationships.
Zeinab Bakhshizarrinabadi, MD, Elie chahla, MD. P2429 - Eosinophilic Gastroenterocolitis in an Elderly Patient Presented With Persistent Diarrhea, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
