Monday Poster Session
Category: General Endoscopy
P2433 - Afferent Limb Small Bowel Obstruction Secondary to Enterolithiasis After Afferent Limb Diverticulitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Fangfang Wang, MD
Mayo Clinic Arizona
Scottsdale, AZ
Presenting Author(s)
Fangfang Wang, MD1, Mashal Batheja, MD2
1Mayo Clinic Arizona, Scottsdale, AZ; 2Mayo Clinic, Phoenix, AZ
Introduction: Enterolithiasis is a rare condition with serious complications. It can form in surgical enteroanastomoses, blind pouches, hernias, small intestinal tumors, inflammatory bowel disease strictures, and intestinal tuberculosis. Small bowel diverticulosis is a significant risk factor. Clinical presentation varies with enterolith location.
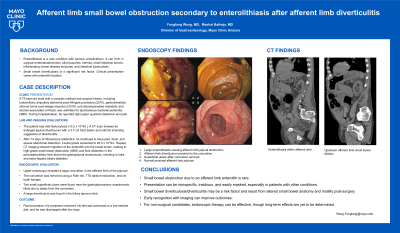
Case Description/Methods: A 75-year-old male with a complex medical and surgical history, including tubulovillous ampullary adenoma post-Whipple procedure (2010), gastrointestinal stromal tumor post-wedge resection (2019), and decompensated metabolic and alcohol-associated cirrhosis, was admitted for spontaneous bacterial peritonitis (SBP). During hospitalization, he reported right upper quadrant distention and pain. The patient had mild leukocytosis (10.2 x 10^9/L). A CT scan showed an enlarged jejunal diverticulum with a 3.7 cm food debris and mild fat stranding suggestive of diverticulitis. Endoscopic evaluation was deferred due to diverticulitis, and broad-spectrum antibiotics were recommended. After 14 days of intravenous antibiotics, he continued to have pain, fever, and severe abdominal distention. Leukocytosis worsened to 20.4 x 10^9/L. Repeat CT imaging showed migration of the enterolith into the bowel lumen, leading to high-grade small bowel obstruction (SBO) and fluid distention in the pancreaticobiliary limb above the gastrojejunal anastomosis, resulting in intra- and extra-hepatic biliary dilatation. Given his comorbidities and preferences, endoscopic therapy was recommended. Upper endoscopy revealed a large concretion in the afferent limb of the jejunum. The concretion was removed using a Roth net, TTS balloon extraction, and rat tooth forceps. Two small superficial ulcers were found near the gastrojejunostomy anastomosis, likely due to stasis from the concretion. A large diverticulum was found in the biliary jejunum limb. Post-procedure, his symptoms resolved, his diet was advanced to a low-residue diet, and he was discharged after two days.
Discussion: Small bowel obstruction due to an afferent limb enterolith is rare. Presentation can be nonspecific, insidious, and easily masked, especially in patients with other conditions. Small bowel diverticulosis/diverticulitis may be a risk factor and result from altered small bowel anatomy and motility post-surgery. Early recognition with imaging can improve outcomes. For non-surgical candidates, endoscopic therapy can be effective, though long-term effects are yet to be determined.

Disclosures:
Fangfang Wang, MD1, Mashal Batheja, MD2. P2433 - Afferent Limb Small Bowel Obstruction Secondary to Enterolithiasis After Afferent Limb Diverticulitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic Arizona, Scottsdale, AZ; 2Mayo Clinic, Phoenix, AZ
Introduction: Enterolithiasis is a rare condition with serious complications. It can form in surgical enteroanastomoses, blind pouches, hernias, small intestinal tumors, inflammatory bowel disease strictures, and intestinal tuberculosis. Small bowel diverticulosis is a significant risk factor. Clinical presentation varies with enterolith location.
Case Description/Methods: A 75-year-old male with a complex medical and surgical history, including tubulovillous ampullary adenoma post-Whipple procedure (2010), gastrointestinal stromal tumor post-wedge resection (2019), and decompensated metabolic and alcohol-associated cirrhosis, was admitted for spontaneous bacterial peritonitis (SBP). During hospitalization, he reported right upper quadrant distention and pain. The patient had mild leukocytosis (10.2 x 10^9/L). A CT scan showed an enlarged jejunal diverticulum with a 3.7 cm food debris and mild fat stranding suggestive of diverticulitis. Endoscopic evaluation was deferred due to diverticulitis, and broad-spectrum antibiotics were recommended. After 14 days of intravenous antibiotics, he continued to have pain, fever, and severe abdominal distention. Leukocytosis worsened to 20.4 x 10^9/L. Repeat CT imaging showed migration of the enterolith into the bowel lumen, leading to high-grade small bowel obstruction (SBO) and fluid distention in the pancreaticobiliary limb above the gastrojejunal anastomosis, resulting in intra- and extra-hepatic biliary dilatation. Given his comorbidities and preferences, endoscopic therapy was recommended. Upper endoscopy revealed a large concretion in the afferent limb of the jejunum. The concretion was removed using a Roth net, TTS balloon extraction, and rat tooth forceps. Two small superficial ulcers were found near the gastrojejunostomy anastomosis, likely due to stasis from the concretion. A large diverticulum was found in the biliary jejunum limb. Post-procedure, his symptoms resolved, his diet was advanced to a low-residue diet, and he was discharged after two days.
Discussion: Small bowel obstruction due to an afferent limb enterolith is rare. Presentation can be nonspecific, insidious, and easily masked, especially in patients with other conditions. Small bowel diverticulosis/diverticulitis may be a risk factor and result from altered small bowel anatomy and motility post-surgery. Early recognition with imaging can improve outcomes. For non-surgical candidates, endoscopic therapy can be effective, though long-term effects are yet to be determined.

Figure: 1. Large enterolithiasis causing afferent limb jejunal obstruction
2. Afferent limb diverticulum proximal to the concretion
3. Superficial ulcers after concretion removal
4. Normal proximal afferent limb jejunum
5. Enterolithiasis within afferent limb
6. Upstream afferent limb small bowel dilation
2. Afferent limb diverticulum proximal to the concretion
3. Superficial ulcers after concretion removal
4. Normal proximal afferent limb jejunum
5. Enterolithiasis within afferent limb
6. Upstream afferent limb small bowel dilation
Disclosures:
Fangfang Wang indicated no relevant financial relationships.
Mashal Batheja indicated no relevant financial relationships.
Fangfang Wang, MD1, Mashal Batheja, MD2. P2433 - Afferent Limb Small Bowel Obstruction Secondary to Enterolithiasis After Afferent Limb Diverticulitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
