Monday Poster Session
Category: GI Bleeding
P2496 - Gastroduodenal Artery Pseudoaneurysm as a Cause of Massive Upper GI Bleeding Decades After Partial Gastrectomy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Hussam Almasri, MD, MRCP
University of North Dakota
Fargo, ND
Presenting Author(s)
Hussam Almasri, MD, MRCP1, Arman Quraishi, MD2, Guneet Sidhu, MD1, John Bassett, MD, FACG3
1University of North Dakota, Fargo, ND; 2University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 3Sanford Health, Fargo, ND
Introduction: Gastroduodenal artery (GDA) pseudoaneurysm is a rare complication of gastric, pancreatic surgery, and severe pancreatitis as well. The presentation is often severe GI bleeding with up to 90% mortality rate. Proper identification of past gastrectomy either based on history or endoscopic appearance is essential to keep GDA in mind and promptly direct individuals toward embolization or surgical intervention, as endoscopic treatments frequently prove ineffective. We present a case of massive GI bleeding linked to having a GDA pseudoaneurysm.
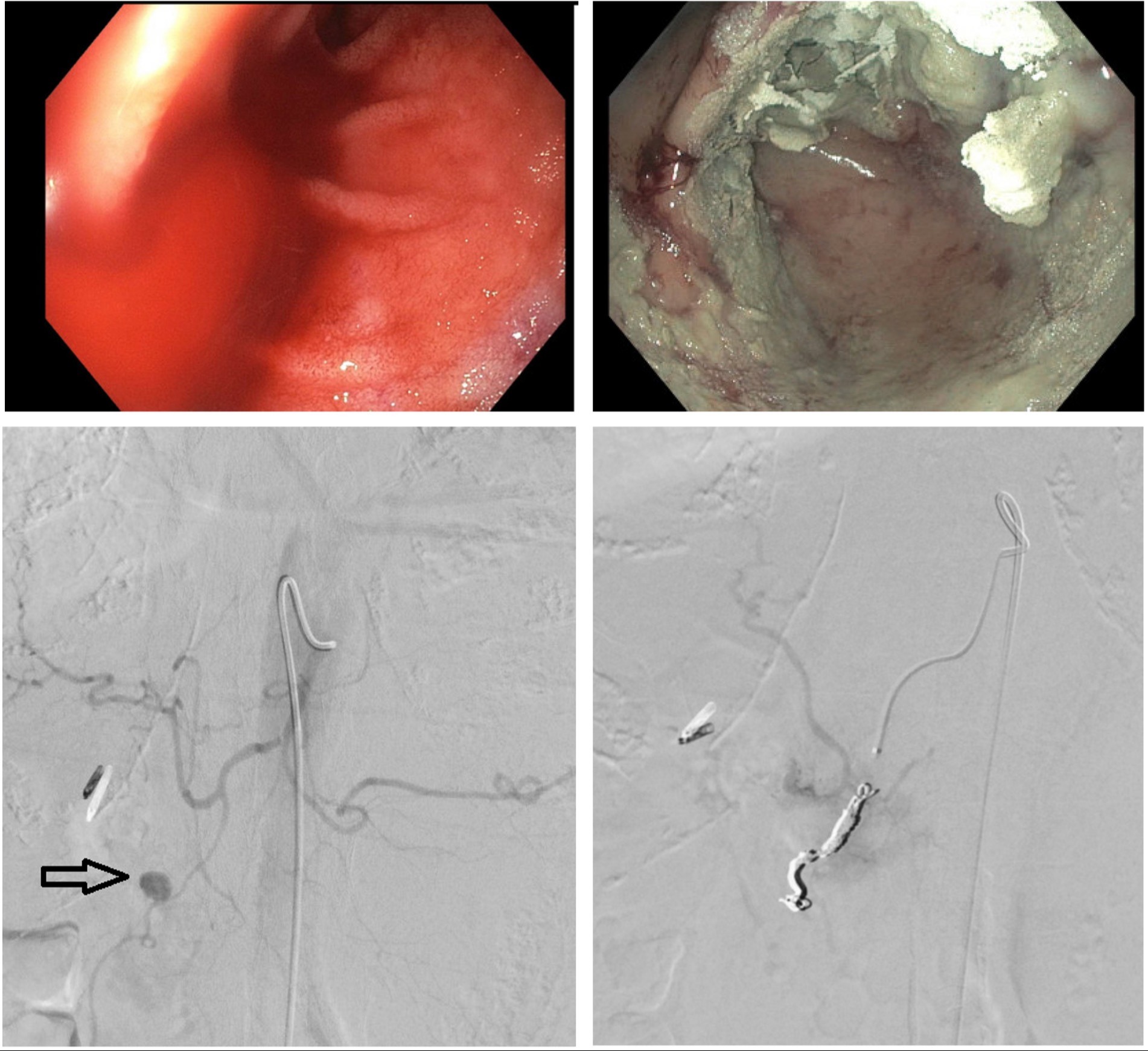
Case Description/Methods: Case-65Y male who had a history of hypertension gastric ulcer-related surgery without clear documentation. There is no history of significant alcohol intake or use of NSAIDs. He presented with hematemesis, black stools, and syncope. The patient was found to be hemodynamically unstable with a heart rate of 120/minute, and blood pressure of 98/66 mmgh. On examination, the abdomen was soft and non-tender. Hemoglobin 8.5 g/dl (baseline 13.8), platelets 235 K/uL creatinine 0.77 mg/dl and INR 1.2. The patient was appropriately resuscitated and an upper endoscopy showed signs of gastroenterostomy with stenosis and duodenal ulcer with spurting hemorrhage (Forrest Class Ia). Despite the administration of adrenaline injection, the bleeding persisted until bipolar cautery, clip placement, and hemostatic spray were employed. Care was continued in the intensive care unit. A recurrence of massive GI bleeding was observed 2 days after endoscopy and the massive transfusion protocol was initiated. IR conducted a Celiac arteriogram, revealing a pseudoaneurysm originating from the gastroduodenal artery (Fig 1). Subsequently, successful embolization was carried out using a helical coil. GI bleeding stopped and the patient's condition stabilized.
Discussion: GI bleeding can be life-threatening. However, early detection and management can reduce this risk. GDA pseudoaneurysm-related bleeding should always be considered in patients who have undergone gastrectomy, bypass surgery, or pancreatectomy. Endoscopic procedures are typically transient and can only provide anatomical correlation before angiography and embolization provide a definitive therapy. Patients with GDA pseudoaneurysm can remain fully asymptomatic for a long period. The most common site of bleeding is the duodenum. If an angiography fails to halt the bleeding, surgical procedures may be considered. The aneurysmal sac is resected during surgery, which can be performed laparoscopically or open.
Disclosures:
Hussam Almasri, MD, MRCP1, Arman Quraishi, MD2, Guneet Sidhu, MD1, John Bassett, MD, FACG3. P2496 - Gastroduodenal Artery Pseudoaneurysm as a Cause of Massive Upper GI Bleeding Decades After Partial Gastrectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Dakota, Fargo, ND; 2University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 3Sanford Health, Fargo, ND
Introduction: Gastroduodenal artery (GDA) pseudoaneurysm is a rare complication of gastric, pancreatic surgery, and severe pancreatitis as well. The presentation is often severe GI bleeding with up to 90% mortality rate. Proper identification of past gastrectomy either based on history or endoscopic appearance is essential to keep GDA in mind and promptly direct individuals toward embolization or surgical intervention, as endoscopic treatments frequently prove ineffective. We present a case of massive GI bleeding linked to having a GDA pseudoaneurysm.
Case Description/Methods: Case-65Y male who had a history of hypertension gastric ulcer-related surgery without clear documentation. There is no history of significant alcohol intake or use of NSAIDs. He presented with hematemesis, black stools, and syncope. The patient was found to be hemodynamically unstable with a heart rate of 120/minute, and blood pressure of 98/66 mmgh. On examination, the abdomen was soft and non-tender. Hemoglobin 8.5 g/dl (baseline 13.8), platelets 235 K/uL creatinine 0.77 mg/dl and INR 1.2. The patient was appropriately resuscitated and an upper endoscopy showed signs of gastroenterostomy with stenosis and duodenal ulcer with spurting hemorrhage (Forrest Class Ia). Despite the administration of adrenaline injection, the bleeding persisted until bipolar cautery, clip placement, and hemostatic spray were employed. Care was continued in the intensive care unit. A recurrence of massive GI bleeding was observed 2 days after endoscopy and the massive transfusion protocol was initiated. IR conducted a Celiac arteriogram, revealing a pseudoaneurysm originating from the gastroduodenal artery (Fig 1). Subsequently, successful embolization was carried out using a helical coil. GI bleeding stopped and the patient's condition stabilized.
Discussion: GI bleeding can be life-threatening. However, early detection and management can reduce this risk. GDA pseudoaneurysm-related bleeding should always be considered in patients who have undergone gastrectomy, bypass surgery, or pancreatectomy. Endoscopic procedures are typically transient and can only provide anatomical correlation before angiography and embolization provide a definitive therapy. Patients with GDA pseudoaneurysm can remain fully asymptomatic for a long period. The most common site of bleeding is the duodenum. If an angiography fails to halt the bleeding, surgical procedures may be considered. The aneurysmal sac is resected during surgery, which can be performed laparoscopically or open.
Figure: Figure 1. A: An endoscopic appearance of the bleeding site (Spurting). B: Post endotherapy. C: Celiac angiogram showing GDA aneurysm. D: Angiogram post coiling.
Disclosures:
Hussam Almasri indicated no relevant financial relationships.
Arman Quraishi indicated no relevant financial relationships.
Guneet Sidhu indicated no relevant financial relationships.
John Bassett indicated no relevant financial relationships.
Hussam Almasri, MD, MRCP1, Arman Quraishi, MD2, Guneet Sidhu, MD1, John Bassett, MD, FACG3. P2496 - Gastroduodenal Artery Pseudoaneurysm as a Cause of Massive Upper GI Bleeding Decades After Partial Gastrectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
