Monday Poster Session
Category: GI Bleeding
P2499 - Colonic Tuberculosis: A Rare Etiology of Anemia Unveiled
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- FM
Faisal Mehmood, MD
HonorHealth
Scottsdale, AZ
Presenting Author(s)
Tanya Hsiung, BS1, Faisal Mehmood, MD2, Joseph Fares, MD2
1Midwestern University, Glendale, AZ; 2HonorHealth, Scottsdale, AZ
Introduction: Extrapulmonary tuberculosis (TB) accounts for 1-3% of all TB cases worldwide. Gastrointestinal (GI) TB more commonly affects immunocompromised patients. It can present with abdominal pain, appetite loss, weight loss, fever, bleeding per rectum, changes in bowel patterns, or anemia. Diagnosis is confirmed on histopathology showing non-caseating granuloma and chronic inflammation with AFB-positive stains.
Case Description/Methods: A 60-year-old male who immigrated from Mexico presented to the hospital with a 3-month history of generalized weakness, abdominal pain with dark stools and bright red blood, anorexia, and 30 lb. unintentional weight loss. He denied having any recent sick contacts. He was not taking NSAIDs or anticoagulants. He had a 10-year history of polymyositis and was taking prednisone 20mg daily. His family history was unremarkable. He appeared cachectic and pale on examination. BMI was 17. A pulmonary exam revealed rhonchi bilaterally in both upper lungs. He had generalized abdominal tenderness without any palpable masses.
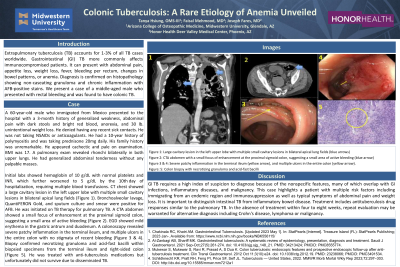
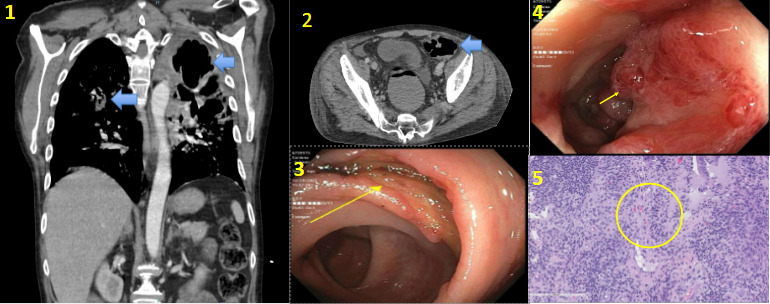
Initial labs showed hemoglobin of 10 g/dL with normal platelets and INR, which further worsened to 5 g/dL by the 10th day of hospitalization, requiring multiple blood transfusions. CT chest showed a large cavitary lesion in the left upper lobe with multiple small cavitary lesions in bilateral apical lung fields (Figure 1). Bronchoalveolar lavage, Quantiferon Gold, and sputum culture and smear were positive for AFB. He was initiated on TB therapy for pulmonary TB. A CTA abdomen showed a small focus of enhancement at the proximal sigmoid colon, suggesting a small area of active bleeding (Figure 2). EGD showed mild erythema in the gastric antrum and duodenum. A colonoscopy revealed severe patchy inflammation in the terminal ileum, and multiple ulcers in the entire colon with no stigmata of recent bleeding (Figure 3 & 4). Biopsy confirmed necrotizing granuloma and acid-fast bacilli within biopsied specimens from the terminal ileum and right-sided colon (Figure 5).
Discussion: GI TB requires a high index of suspicion to diagnose because of the nonspecific features, many of which overlap with GI infections, inflammatory diseases, and malignancy. This case highlights a patient with multiple risk factors including immigrating from an endemic region and immunosuppression as well as typical symptoms of abdominal pain and weight loss.
Disclosures:
Tanya Hsiung, BS1, Faisal Mehmood, MD2, Joseph Fares, MD2. P2499 - Colonic Tuberculosis: A Rare Etiology of Anemia Unveiled, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Midwestern University, Glendale, AZ; 2HonorHealth, Scottsdale, AZ
Introduction: Extrapulmonary tuberculosis (TB) accounts for 1-3% of all TB cases worldwide. Gastrointestinal (GI) TB more commonly affects immunocompromised patients. It can present with abdominal pain, appetite loss, weight loss, fever, bleeding per rectum, changes in bowel patterns, or anemia. Diagnosis is confirmed on histopathology showing non-caseating granuloma and chronic inflammation with AFB-positive stains.
Case Description/Methods: A 60-year-old male who immigrated from Mexico presented to the hospital with a 3-month history of generalized weakness, abdominal pain with dark stools and bright red blood, anorexia, and 30 lb. unintentional weight loss. He denied having any recent sick contacts. He was not taking NSAIDs or anticoagulants. He had a 10-year history of polymyositis and was taking prednisone 20mg daily. His family history was unremarkable. He appeared cachectic and pale on examination. BMI was 17. A pulmonary exam revealed rhonchi bilaterally in both upper lungs. He had generalized abdominal tenderness without any palpable masses.
Initial labs showed hemoglobin of 10 g/dL with normal platelets and INR, which further worsened to 5 g/dL by the 10th day of hospitalization, requiring multiple blood transfusions. CT chest showed a large cavitary lesion in the left upper lobe with multiple small cavitary lesions in bilateral apical lung fields (Figure 1). Bronchoalveolar lavage, Quantiferon Gold, and sputum culture and smear were positive for AFB. He was initiated on TB therapy for pulmonary TB. A CTA abdomen showed a small focus of enhancement at the proximal sigmoid colon, suggesting a small area of active bleeding (Figure 2). EGD showed mild erythema in the gastric antrum and duodenum. A colonoscopy revealed severe patchy inflammation in the terminal ileum, and multiple ulcers in the entire colon with no stigmata of recent bleeding (Figure 3 & 4). Biopsy confirmed necrotizing granuloma and acid-fast bacilli within biopsied specimens from the terminal ileum and right-sided colon (Figure 5).
Discussion: GI TB requires a high index of suspicion to diagnose because of the nonspecific features, many of which overlap with GI infections, inflammatory diseases, and malignancy. This case highlights a patient with multiple risk factors including immigrating from an endemic region and immunosuppression as well as typical symptoms of abdominal pain and weight loss.
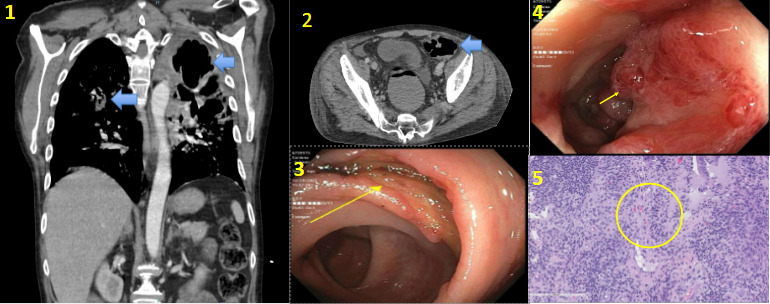
Figure: Figure 1: Large cavitary lesion in the left upper lobe with multiple small cavitary lesions in bilateral apical lung fields (blue arrows)
Figure 2: CTA abdomen with a small focus of enhancement at the proximal sigmoid colon, suggesting a small area of active bleeding (blue arrow)
Figure 3 & 4: Severe patchy inflammation in the terminal ileum (yellow arrow), and multiple ulcers in the entire colon (yellow arrow).
Figure: 5: Colon biopsy with necrotizing granuloma and acid-fast bacilli
Figure 2: CTA abdomen with a small focus of enhancement at the proximal sigmoid colon, suggesting a small area of active bleeding (blue arrow)
Figure 3 & 4: Severe patchy inflammation in the terminal ileum (yellow arrow), and multiple ulcers in the entire colon (yellow arrow).
Figure: 5: Colon biopsy with necrotizing granuloma and acid-fast bacilli
Disclosures:
Tanya Hsiung indicated no relevant financial relationships.
Faisal Mehmood indicated no relevant financial relationships.
Joseph Fares indicated no relevant financial relationships.
Tanya Hsiung, BS1, Faisal Mehmood, MD2, Joseph Fares, MD2. P2499 - Colonic Tuberculosis: A Rare Etiology of Anemia Unveiled, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
