Monday Poster Session
Category: GI Bleeding
P2507 - Gastric Multiple Myeloma: An Unusual Cause of Upper GI Bleeding
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JJ
Joel Joseph, MD
Virginia Tech Carilion School of Medicine
Roanoke, VA
Presenting Author(s)
Noel Puthenveetil, MD1, Nathan Puthenveetil, MS2, Joel Joseph, MD3
1OSF Saint Francis Medical Center, Galesburg, IL; 2Loyola University Chicago Stritch School of Medicine, Galesburg, IL; 3Virginia Tech Carilion School of Medicine, Roanoke, VA
Introduction: Multiple myeloma (MM) is a neoplasm arising from malignant transformation of plasma cells, accounting for up to 1 in 10 hematologic cancers. The hallmark of MM is organ dysfunction, including hypercalcemia, renal insufficiency, anemia, and skeletal lesions. However, gastrointestinal (GI) tract involvement is much less common, documented in fewer than 5% of cases. GI symptoms range from diarrhea to overt bowel obstruction.
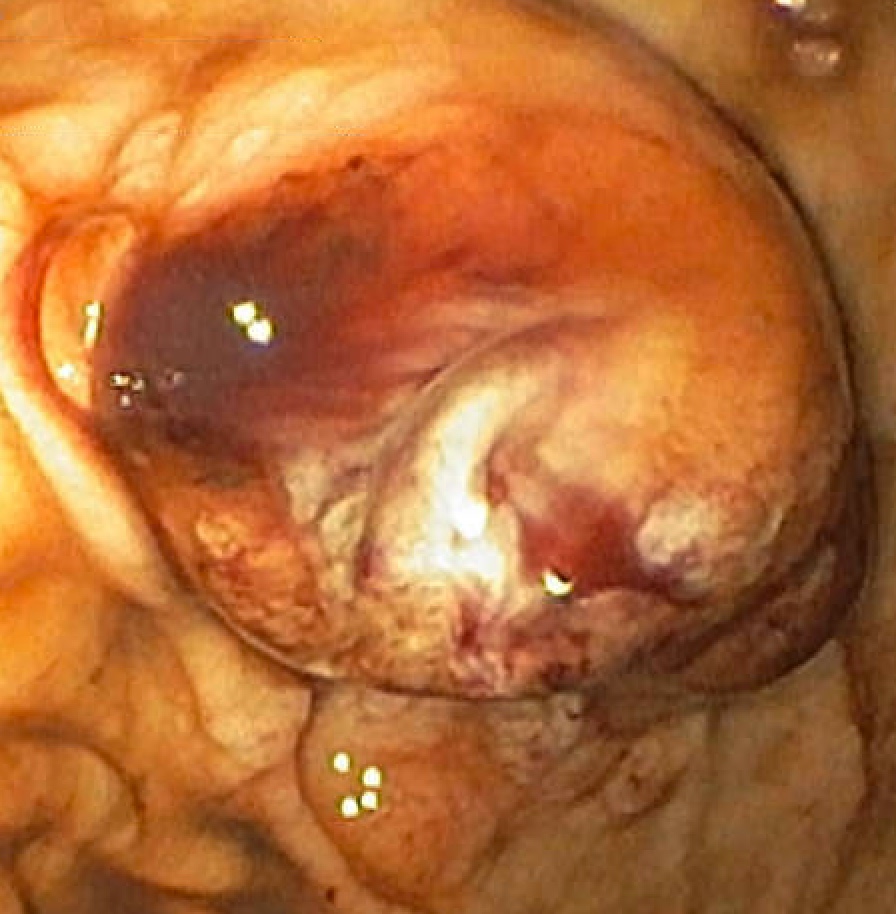
Case Description/Methods: We present the case of a 76-year-old male with a history of hypertension, type 2 diabetes, and multiple myeloma with multiple bony lesions, most recently treated with daratumumab and pomalidomide. He presented to the emergency department with melena and weakness. On arrival, he was tachycardic at 110 beats per minute but otherwise hemodynamically stable. Initial labs showed hemoglobin of 7.5 g/dL (down from 13.3 two months prior), with normal platelets (212,000) and international normalized ratio (1.0). An upper endoscopy performed on arrival revealed an actively oozing 8 mm cratered lesion with heaped margins on the lesser curvature of the stomach, managed with a combination of epinephrine, 3 Hemoclips, and Hemospray achieving initial hemostasis. However, he experienced further episodes of melena and underwent repeat endoscopy three days later, which revealed ongoing oozing from the gastric lesion, necessitating deployment of an additional 2 Hemoclips. Cold forcep biopsies were obtained from the edges and center of the lesion, with pathology showing atypical CD138-positive cells indicative of plasma cell differentiation. Subsequent in situ hybridization testing confirmed lambda restriction. Due to concern for multiple myeloma involvement in this bleeding gastric ulceration, he underwent one round of palliative radiation. His clinical course was complicated by respiratory distress from a large malignant pleural effusion, and he was transitioned to comfort care before passing away on hospital day 7.
Discussion: This case highlights an atypical presentation of multiple myeloma causing upper GI bleeding. In addition to neoplastic ulceration, bleeding in these patients can be compounded by clotting abnormalities due to neoplastic bone marrow involvement. Although gastric myeloma is exceedingly rare, its presence indicates an overall poor prognosis. Understanding the extramedullary manifestations of MM is crucial for accurate diagnosis and timely treatment.
Disclosures:
Noel Puthenveetil, MD1, Nathan Puthenveetil, MS2, Joel Joseph, MD3. P2507 - Gastric Multiple Myeloma: An Unusual Cause of Upper GI Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1OSF Saint Francis Medical Center, Galesburg, IL; 2Loyola University Chicago Stritch School of Medicine, Galesburg, IL; 3Virginia Tech Carilion School of Medicine, Roanoke, VA
Introduction: Multiple myeloma (MM) is a neoplasm arising from malignant transformation of plasma cells, accounting for up to 1 in 10 hematologic cancers. The hallmark of MM is organ dysfunction, including hypercalcemia, renal insufficiency, anemia, and skeletal lesions. However, gastrointestinal (GI) tract involvement is much less common, documented in fewer than 5% of cases. GI symptoms range from diarrhea to overt bowel obstruction.
Case Description/Methods: We present the case of a 76-year-old male with a history of hypertension, type 2 diabetes, and multiple myeloma with multiple bony lesions, most recently treated with daratumumab and pomalidomide. He presented to the emergency department with melena and weakness. On arrival, he was tachycardic at 110 beats per minute but otherwise hemodynamically stable. Initial labs showed hemoglobin of 7.5 g/dL (down from 13.3 two months prior), with normal platelets (212,000) and international normalized ratio (1.0). An upper endoscopy performed on arrival revealed an actively oozing 8 mm cratered lesion with heaped margins on the lesser curvature of the stomach, managed with a combination of epinephrine, 3 Hemoclips, and Hemospray achieving initial hemostasis. However, he experienced further episodes of melena and underwent repeat endoscopy three days later, which revealed ongoing oozing from the gastric lesion, necessitating deployment of an additional 2 Hemoclips. Cold forcep biopsies were obtained from the edges and center of the lesion, with pathology showing atypical CD138-positive cells indicative of plasma cell differentiation. Subsequent in situ hybridization testing confirmed lambda restriction. Due to concern for multiple myeloma involvement in this bleeding gastric ulceration, he underwent one round of palliative radiation. His clinical course was complicated by respiratory distress from a large malignant pleural effusion, and he was transitioned to comfort care before passing away on hospital day 7.
Discussion: This case highlights an atypical presentation of multiple myeloma causing upper GI bleeding. In addition to neoplastic ulceration, bleeding in these patients can be compounded by clotting abnormalities due to neoplastic bone marrow involvement. Although gastric myeloma is exceedingly rare, its presence indicates an overall poor prognosis. Understanding the extramedullary manifestations of MM is crucial for accurate diagnosis and timely treatment.
Figure: Bleeding gastric mass with central ulceration
Disclosures:
Noel Puthenveetil indicated no relevant financial relationships.
Nathan Puthenveetil indicated no relevant financial relationships.
Joel Joseph indicated no relevant financial relationships.
Noel Puthenveetil, MD1, Nathan Puthenveetil, MS2, Joel Joseph, MD3. P2507 - Gastric Multiple Myeloma: An Unusual Cause of Upper GI Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
