Monday Poster Session
Category: GI Bleeding
P2533 - Atraumatic Splenic Hemorrhage Post Acute Alcoholic Necrotizing Pancreatitis: A Case Report
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Obada Daaboul, MD
Southern Illinois University
Springfield, IL
Presenting Author(s)
Zeyad J. Rifai, DO, Mohamad Hekmat Sukkari, MD, Obada Daaboul, MD, Tasnem Alsebai, MD, Mulham Alom, MD
Southern Illinois University, Springfield, IL
Introduction: Atraumatic splenic hemorrhage is an uncommon but life-threatening condition that requires immediate intervention. The incidence of this rare condition is poorly documented in the literature, particularly when acute pancreatitis is the etiology of the splenic hemorrhage. We present a rare case of atraumatic splenic hemorrhage as a complication of acute alcoholic necrotizing pancreatitis requiring coil embolization of the upper and lower pole splenic arteries. We aim to highlight the importance of considering splenic hemorrhage as a differential diagnosis in patients with acute abdominal pain, particularly in the setting of acute pancreatitis.
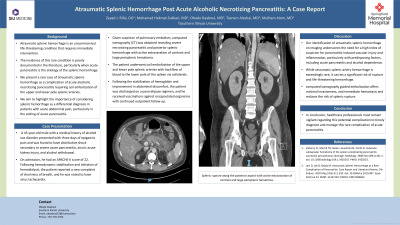
Case Description/Methods: 43-year-old male with a medical history of alcohol use disorder presented with three days of epigastric pain and was found to have distributive shock secondary to severe acute pancreatitis, anuric acute kidney injury, and alcohol withdrawal. On admission, he had an APACHE-II score of 22. Following hemodynamic stabilization and initiation of hemodialysis, the patient mentioned a new complaint of shortness of breath and had noted sinus tachycardia. Given suspicion for pulmonary embolism, computed tomography (CT) was obtained revealing severe necrotizing pancreatitis and posterior splenic hemorrhage with active extravasation of contrast and large perisplenic hematoma. The patient underwent coil embolization of the upper and lower pole splenic arteries with backflow of blood to the lower pole of the spleen via collaterals. He was started on Ampicillin-Sulbactam for prophylaxis against splenic abscess and received vaccination against encapsulated organisms. Following stabilization of hemoglobin and improvement in abdominal discomfort, the patient was discharged on a pancrelipase regimen with continued outpatient follow-up.
Discussion: Our identification of atraumatic splenic hemorrhage on imaging underscores the need for a high index of suspicion for pancreatitis-induced vascular injury and inflammation, particularly with predisposing factors, including acute pancreatitis and alcohol dependence. While atraumatic splenic artery hemorrhage is exceedingly rare, it carries a significant risk of rupture and life-threatening hemorrhage. Image-guided embolization offers minimal invasiveness, immediate hemostasis and reduces risk of splenic rupture. Healthcare professionals must remain vigilant regarding this potential complication to timely diagnose and manage this rare complication of acute pancreatitis.

Disclosures:
Zeyad J. Rifai, DO, Mohamad Hekmat Sukkari, MD, Obada Daaboul, MD, Tasnem Alsebai, MD, Mulham Alom, MD. P2533 - Atraumatic Splenic Hemorrhage Post Acute Alcoholic Necrotizing Pancreatitis: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Southern Illinois University, Springfield, IL
Introduction: Atraumatic splenic hemorrhage is an uncommon but life-threatening condition that requires immediate intervention. The incidence of this rare condition is poorly documented in the literature, particularly when acute pancreatitis is the etiology of the splenic hemorrhage. We present a rare case of atraumatic splenic hemorrhage as a complication of acute alcoholic necrotizing pancreatitis requiring coil embolization of the upper and lower pole splenic arteries. We aim to highlight the importance of considering splenic hemorrhage as a differential diagnosis in patients with acute abdominal pain, particularly in the setting of acute pancreatitis.
Case Description/Methods: 43-year-old male with a medical history of alcohol use disorder presented with three days of epigastric pain and was found to have distributive shock secondary to severe acute pancreatitis, anuric acute kidney injury, and alcohol withdrawal. On admission, he had an APACHE-II score of 22. Following hemodynamic stabilization and initiation of hemodialysis, the patient mentioned a new complaint of shortness of breath and had noted sinus tachycardia. Given suspicion for pulmonary embolism, computed tomography (CT) was obtained revealing severe necrotizing pancreatitis and posterior splenic hemorrhage with active extravasation of contrast and large perisplenic hematoma. The patient underwent coil embolization of the upper and lower pole splenic arteries with backflow of blood to the lower pole of the spleen via collaterals. He was started on Ampicillin-Sulbactam for prophylaxis against splenic abscess and received vaccination against encapsulated organisms. Following stabilization of hemoglobin and improvement in abdominal discomfort, the patient was discharged on a pancrelipase regimen with continued outpatient follow-up.
Discussion: Our identification of atraumatic splenic hemorrhage on imaging underscores the need for a high index of suspicion for pancreatitis-induced vascular injury and inflammation, particularly with predisposing factors, including acute pancreatitis and alcohol dependence. While atraumatic splenic artery hemorrhage is exceedingly rare, it carries a significant risk of rupture and life-threatening hemorrhage. Image-guided embolization offers minimal invasiveness, immediate hemostasis and reduces risk of splenic rupture. Healthcare professionals must remain vigilant regarding this potential complication to timely diagnose and manage this rare complication of acute pancreatitis.

Figure: Coronal view of splenic hemorrhage prior to embolization
Disclosures:
Zeyad Rifai indicated no relevant financial relationships.
Mohamad Hekmat Sukkari indicated no relevant financial relationships.
Obada Daaboul indicated no relevant financial relationships.
Tasnem Alsebai indicated no relevant financial relationships.
Mulham Alom indicated no relevant financial relationships.
Zeyad J. Rifai, DO, Mohamad Hekmat Sukkari, MD, Obada Daaboul, MD, Tasnem Alsebai, MD, Mulham Alom, MD. P2533 - Atraumatic Splenic Hemorrhage Post Acute Alcoholic Necrotizing Pancreatitis: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
