Monday Poster Session
Category: GI Bleeding
P2536 - A Rare Cause of GI Bleeding: Concurrent Kaposi Sarcoma and CMV Infection
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CM
Cesar Moreno, MD
USA Health, University of South Alabama
Mobile, AL
Presenting Author(s)
Cesar Moreno, MD1, David Engerson, MD2, Charu Shastri, MD2, Rajab Idriss, MD2
1USA Health, University of South Alabama, Mobile, AL; 2University of South Alabama, Mobile, AL
Introduction: Gastrointestinal (GI) bleeding in patients with Acquired Immunodeficiency Syndrome (AIDS) is uncommon and can be caused by AIDS-related opportunistic infections or neoplasms. Small bowel bleeding occurs in approximately 5-10% of all cases in the general population. The incidence of small bowel bleeding in the AIDS population is exceedingly rare. We present the case of a 39-year-old male with AIDS and small bowel bleeding due to Kaposi sarcoma (KS) and cytomegalovirus (CMV) infection.
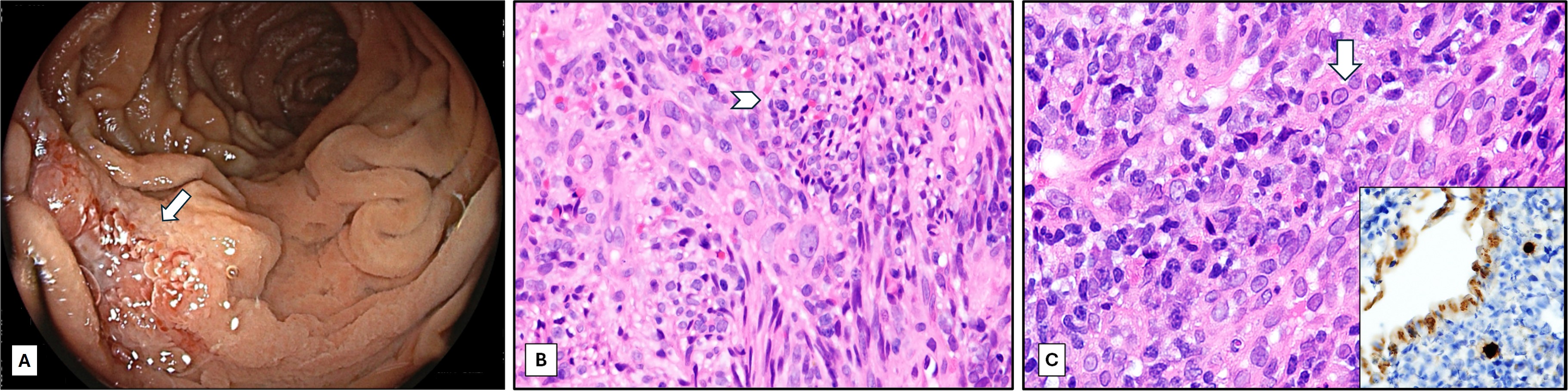
Case Description/Methods: A 39 year-old male with AIDS and antiretroviral therapy non-compliance was admitted to the intensive care unit due to syncope, severe anemia and melena. Exam showed an ill-appearing male with multiple plaque-like violaceous lesions over his arms and neck. Laboratory evaluation revealed hemoglobin 3 g/dL, lactate 11 mmol/L, absolute CD4 count of 5 cells/mcL. Patient had marked clinical improvement after transfusion of 5 units of red blood cells. Inpatient bidirectional endoscopy was unremarkable. Follow up video capsule endoscopy showed several malignant appearing lesions in the proximal jejunum at 30% small bowel transit time. Follow up push enteroscopy revealed proximal jejunum ulcers that were positive for KS and CMV (figure 1). Of note, punch biopsy of the patient’s skin lesions revealed cutaneous KS. Patient was restarted on antiretroviral therapy and anti-CMV therapy with increased CD4 count of 108 cells/mcL, no more bleeding episodes, stable hemoglobin, and partial regression of his cutaneous KS.
Discussion: Upper GI bleeding is more common than lower GI bleeding and may be due to non-Human Immunodeficiency Virus associated causes while lower GI bleeding is mainly due to opportunistic infection. Small bowel bleeding in patients with AIDS is rare and may be caused by tumors or opportunistic infections. KS is a vascular tumor caused by human herpesvirus 8. Most small bowel KS remain asymptomatic. CMV is an opportunistic infection that causes mucosal ulceration and bleeding. To our knowledge, this is the first reported case in the literature of small bowel bleeding due to concurrent small bowel Kaposi sarcoma and CMV enteritis. This case highlights the importance of keeping a broad differential to include opportunistic infection and neoplasms when considering GI bleeding in patients with AIDS and unremarkable bidirectional endoscopy.
Disclosures:
Cesar Moreno, MD1, David Engerson, MD2, Charu Shastri, MD2, Rajab Idriss, MD2. P2536 - A Rare Cause of GI Bleeding: Concurrent Kaposi Sarcoma and CMV Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1USA Health, University of South Alabama, Mobile, AL; 2University of South Alabama, Mobile, AL
Introduction: Gastrointestinal (GI) bleeding in patients with Acquired Immunodeficiency Syndrome (AIDS) is uncommon and can be caused by AIDS-related opportunistic infections or neoplasms. Small bowel bleeding occurs in approximately 5-10% of all cases in the general population. The incidence of small bowel bleeding in the AIDS population is exceedingly rare. We present the case of a 39-year-old male with AIDS and small bowel bleeding due to Kaposi sarcoma (KS) and cytomegalovirus (CMV) infection.
Case Description/Methods: A 39 year-old male with AIDS and antiretroviral therapy non-compliance was admitted to the intensive care unit due to syncope, severe anemia and melena. Exam showed an ill-appearing male with multiple plaque-like violaceous lesions over his arms and neck. Laboratory evaluation revealed hemoglobin 3 g/dL, lactate 11 mmol/L, absolute CD4 count of 5 cells/mcL. Patient had marked clinical improvement after transfusion of 5 units of red blood cells. Inpatient bidirectional endoscopy was unremarkable. Follow up video capsule endoscopy showed several malignant appearing lesions in the proximal jejunum at 30% small bowel transit time. Follow up push enteroscopy revealed proximal jejunum ulcers that were positive for KS and CMV (figure 1). Of note, punch biopsy of the patient’s skin lesions revealed cutaneous KS. Patient was restarted on antiretroviral therapy and anti-CMV therapy with increased CD4 count of 108 cells/mcL, no more bleeding episodes, stable hemoglobin, and partial regression of his cutaneous KS.
Discussion: Upper GI bleeding is more common than lower GI bleeding and may be due to non-Human Immunodeficiency Virus associated causes while lower GI bleeding is mainly due to opportunistic infection. Small bowel bleeding in patients with AIDS is rare and may be caused by tumors or opportunistic infections. KS is a vascular tumor caused by human herpesvirus 8. Most small bowel KS remain asymptomatic. CMV is an opportunistic infection that causes mucosal ulceration and bleeding. To our knowledge, this is the first reported case in the literature of small bowel bleeding due to concurrent small bowel Kaposi sarcoma and CMV enteritis. This case highlights the importance of keeping a broad differential to include opportunistic infection and neoplasms when considering GI bleeding in patients with AIDS and unremarkable bidirectional endoscopy.
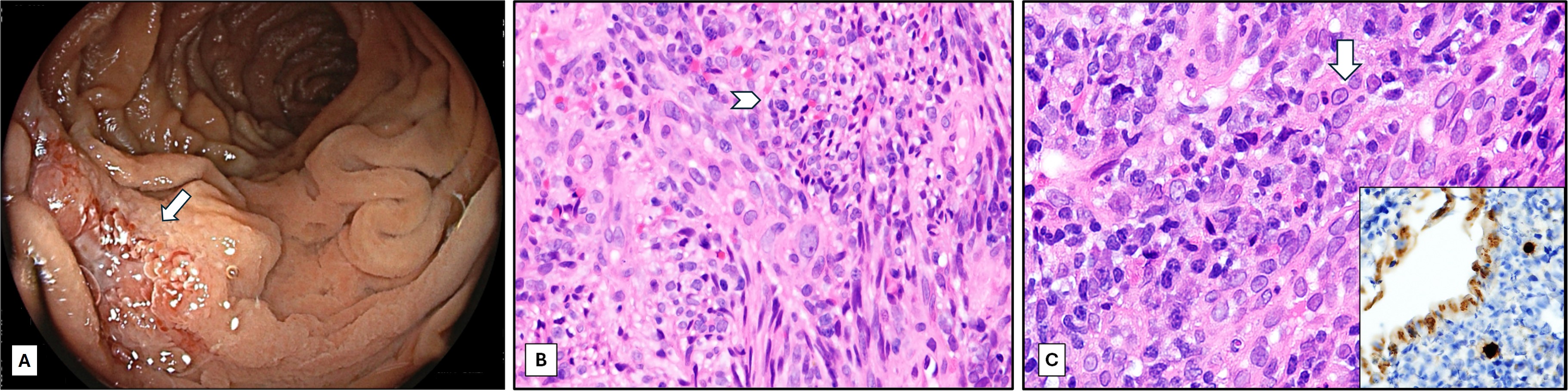
Figure: Panel A. Jejunal ulcer (arrow) found on push enteroscopy. Panel B. Spindle cell proliferation with nuclear atypia and scattered mitotic activity (arrowhead), that expressed CD 31, ERG, and HHV-8 by immunohistochemistry (Hematoxylin and eosin, 400x). These findings support the diagnosis of Kaposi sarcoma. Panel C. Jejunal mucosa showing granulation tissue with viral cytopathic changes (arrow), positive for CMV immunohistochemistry (inset) (Hematoxylin and eosin x400).
Disclosures:
Cesar Moreno indicated no relevant financial relationships.
David Engerson indicated no relevant financial relationships.
Charu Shastri indicated no relevant financial relationships.
Rajab Idriss indicated no relevant financial relationships.
Cesar Moreno, MD1, David Engerson, MD2, Charu Shastri, MD2, Rajab Idriss, MD2. P2536 - A Rare Cause of GI Bleeding: Concurrent Kaposi Sarcoma and CMV Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
