Monday Poster Session
Category: GI Bleeding
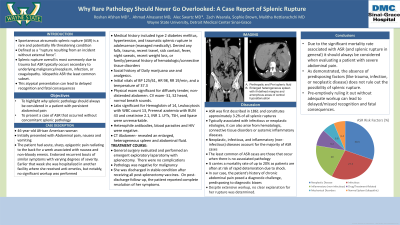
P2538 - Why Rare Pathology Should Never Go Overlooked: A Case Report of Splenic Rupture
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Alec Swartz, BS
Ross University School of Medicine
Detroit, MI
Presenting Author(s)
Roshan Afshan, MDsup>1, Ahmad Alnasarat, MD2, Alec Swartz, MD<3, Zach Waarala, 4, Sophie Brown, 4, Marc Feldman, MD5, Malitha Hettiarachchi, MD5
1Detroit Medical Center, Novi, MI; 2DMC Sinai-Grace Hospital, Farmington Hills, MI; 3Detroit Medical Center, Detroit, MI; 4Wayne State University, Detroit, MI; 5Detroit Medical Center/Wayne State University, Detroit, MI
Introduction: Spontaneous atraumatic splenic rupture (ASR) is an uncommon yet serious condition that is usually infectious or neoplastic in origin. Due to the significant health risks associated with delayed care, prompt evaluation and management are paramount. We report a case of a 46-year-old female with ASR and no identifiable etiology.
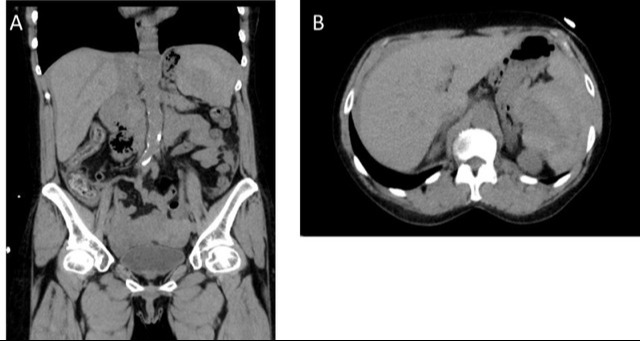
Case Description/Methods: A 46-year-old woman with a history of type 2 diabetes mellitus, hypertension, traumatic splenic rupture in adolescence presented with acute, sharp epigastric pain, radiating to the back, for a week and no relieving factors. It was associated with nausea and non-bloody emesis. She reported having recurrent bouts of similar symptoms with various degrees of severity. She denied any falls, trauma, recent travel, sick contact, fever, night sweats, recent weight loss, or family/personal history of hematologic/connective tissue disorders. Social history was significant for daily marijuana use. Earlier that week she was hospitalized in another facility where she received anti-emetics and analgesics. On exam, the patient was vitally stable with diffusely tender, non-distended abdomen. Labs revealed a Hemoglobin of 14, leukocytosis with WBC count 13, Prerenal azotemia with BUN 43, and creatinine 2.1, INR 1. LFTs, TSH, and lipase were unremarkable. Heterophile antibodies, blood parasites and HIV were negative. Computed Tomography (CT) revealed an enlarged, heterogeneous spleen and abdominal fluid. General surgery evaluated and performed an emergent exploratory laparotomy with splenectomy. Pathology was negative for malignancy. She was discharged in stable condition after receiving all post-splenectomy vaccines. On post-discharge follow-up, the patient reported resolution of her symptoms with a healing surgical scar.
Discussion: ASR was first described in 1861 and constitutes approximately 3.2% cases of all splenic ruptures. Typically associated with infectious or neoplastic etiologies, it can also arise from hematologic, connective tissue disorders or systemic inflammatory diseases. It carries a mortality rate of up to 20%, as patients are often at risk of rapid deterioration due to shock. In our case, the patient's history of chronic abdominal pain posed a diagnostic challenge, predisposing to diagnostic biases. Hence, when evaluating patients with severe abdominal pain it is essential to consider a wide spectrum of differentials including ASR, even in the absence of predisposing factors such as trauma, infectious, or neoplastic conditions.
Disclosures:
Roshan Afshan, MD1, Ahmad Alnasarat, MD2, Alec Swartz, MD3, Zach Waarala, 4, Sophie Brown, 4, Marc Feldman, MD5, Malitha Hettiarachchi, MD5. P2538 - Why Rare Pathology Should Never Go Overlooked: A Case Report of Splenic Rupture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Detroit Medical Center, Novi, MI; 2DMC Sinai-Grace Hospital, Farmington Hills, MI; 3Detroit Medical Center, Detroit, MI; 4Wayne State University, Detroit, MI; 5Detroit Medical Center/Wayne State University, Detroit, MI
Introduction: Spontaneous atraumatic splenic rupture (ASR) is an uncommon yet serious condition that is usually infectious or neoplastic in origin. Due to the significant health risks associated with delayed care, prompt evaluation and management are paramount. We report a case of a 46-year-old female with ASR and no identifiable etiology.
Case Description/Methods: A 46-year-old woman with a history of type 2 diabetes mellitus, hypertension, traumatic splenic rupture in adolescence presented with acute, sharp epigastric pain, radiating to the back, for a week and no relieving factors. It was associated with nausea and non-bloody emesis. She reported having recurrent bouts of similar symptoms with various degrees of severity. She denied any falls, trauma, recent travel, sick contact, fever, night sweats, recent weight loss, or family/personal history of hematologic/connective tissue disorders. Social history was significant for daily marijuana use. Earlier that week she was hospitalized in another facility where she received anti-emetics and analgesics. On exam, the patient was vitally stable with diffusely tender, non-distended abdomen. Labs revealed a Hemoglobin of 14, leukocytosis with WBC count 13, Prerenal azotemia with BUN 43, and creatinine 2.1, INR 1. LFTs, TSH, and lipase were unremarkable. Heterophile antibodies, blood parasites and HIV were negative. Computed Tomography (CT) revealed an enlarged, heterogeneous spleen and abdominal fluid. General surgery evaluated and performed an emergent exploratory laparotomy with splenectomy. Pathology was negative for malignancy. She was discharged in stable condition after receiving all post-splenectomy vaccines. On post-discharge follow-up, the patient reported resolution of her symptoms with a healing surgical scar.
Discussion: ASR was first described in 1861 and constitutes approximately 3.2% cases of all splenic ruptures. Typically associated with infectious or neoplastic etiologies, it can also arise from hematologic, connective tissue disorders or systemic inflammatory diseases. It carries a mortality rate of up to 20%, as patients are often at risk of rapid deterioration due to shock. In our case, the patient's history of chronic abdominal pain posed a diagnostic challenge, predisposing to diagnostic biases. Hence, when evaluating patients with severe abdominal pain it is essential to consider a wide spectrum of differentials including ASR, even in the absence of predisposing factors such as trauma, infectious, or neoplastic conditions.
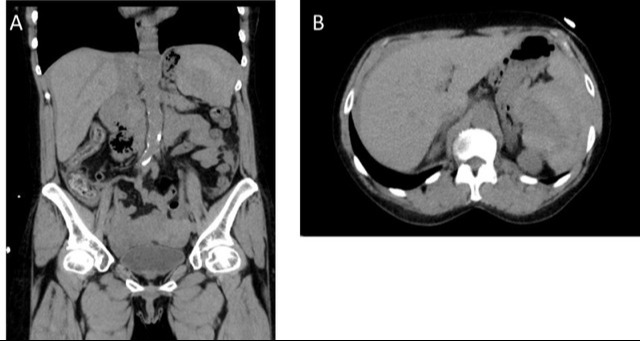
Figure: A. Perihepatic and Peri splenic fluid
B. Enlarged heterogeneous spleen with ill-defined margins and amorphous areas of central hypoattenuation
B. Enlarged heterogeneous spleen with ill-defined margins and amorphous areas of central hypoattenuation
Disclosures:
Roshan Afshan indicated no relevant financial relationships.
Ahmad Alnasarat indicated no relevant financial relationships.
Alec Swartz indicated no relevant financial relationships.
Zach Waarala indicated no relevant financial relationships.
Sophie Brown indicated no relevant financial relationships.
Marc Feldman indicated no relevant financial relationships.
Malitha Hettiarachchi indicated no relevant financial relationships.
Roshan Afshan, MD1, Ahmad Alnasarat, MD2, Alec Swartz, MD3, Zach Waarala, 4, Sophie Brown, 4, Marc Feldman, MD5, Malitha Hettiarachchi, MD5. P2538 - Why Rare Pathology Should Never Go Overlooked: A Case Report of Splenic Rupture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
