Monday Poster Session
Category: GI Bleeding
P2540 - A Life-Threatening Rectal Dieulafoy Lesion Requiring a Multi-Disciplinary Approach
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Rohan Rau, DO
Albert Einstein Medical Center
Philadelphia, PA
Presenting Author(s)
Rohan Rau, DO1, Sanjay Rau, DO2, Kyle Kreitman, DO3
1Albert Einstein Medical Center, Philadelphia, PA; 2University of Massachusetts, Worcester, MA; 3UMass, Worcester, MA
Introduction: Dieulafoy lesions are aberrant vessels that cause significant bleeding without ulcers or erosions. They account for about 5% of acute gastrointestinal (GI) hemorrhages. Typically found on the stomach's lesser curvature, these lesions can occur anywhere in the GI tract, with only 2% in the rectum. We present a rare case of a life-threatening rectal Dieulafoy lesion requiring a multidisciplinary approach.
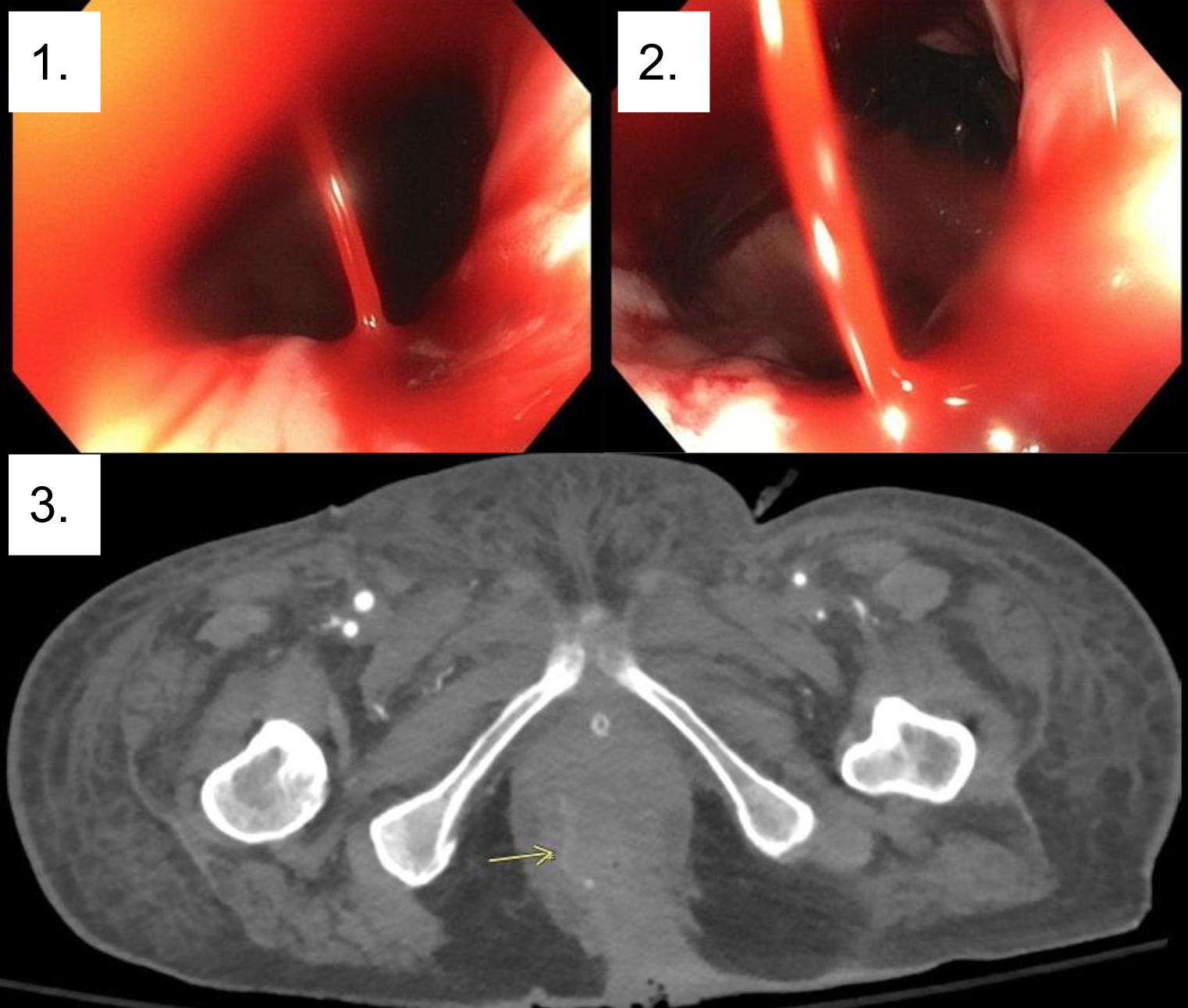
Case Description/Methods: A 73-year-old female with a history of ulcerative colitis, rectal prolapse status post-rectopexy, and coronary artery disease presented after a mechanical fall. The hospital course was complicated by splenic laceration requiring embolization, respiratory failure, fungemia, common femoral artery occlusion requiring thrombectomy, and an abdominal hematoma requiring evacuation. A week into her admission, she developed severe hematochezia becoming tachycardic and hypotensive, necessitating pressors. IV Protonix was started and anticoagulation was held. After resuscitation with blood products, a colonoscopy demonstrated an actively spurting Dieulafoy lesion at the distal rectum 2 cm proximal to the anal verge. Given the location, endoscopic intervention was unable to be performed. Computer Tomography angiogram (CTA) displayed a focal bleed at the inferior rectal artery. Radiology advised against embolization due to its distal location and concerns for causing ischemia. As a result, Colorectal surgery was asked to see the patient. Thrombin-soaked gel foam pads, topical hemostatic agents, and direct pressure were applied initially, followed by direct cauterization to the vessel. Primary hemostasis was achieved and there were no further episodes of rebleeding.
Discussion: Common causes of massive rectal bleeding include hemorrhoids, anal fissures, and fistulas-in-ano, with rectal Dieulafoy lesions being a rare but severe cause. This case highlights the importance of a multidisciplinary approach. Colonoscopy remains the standard for diagnosis and treatment for profuse lower GI bleeding. In this case, direct visualization ruled out other possible causes of lower GI bleed and confirmed an aberrant spurting vessel. Notably, the patient’s post-surgical rectal anatomy, location, and severity of bleeding made endoscopic intervention difficult. When endoscopy and radiologic intervention are limited, surgical evaluation is warranted to intervene. In this case, surgical intervention with manual pressure and mucosal cautery provided definitive hemostasis.
Disclosures:
Rohan Rau, DO1, Sanjay Rau, DO2, Kyle Kreitman, DO3. P2540 - A Life-Threatening Rectal Dieulafoy Lesion Requiring a Multi-Disciplinary Approach, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albert Einstein Medical Center, Philadelphia, PA; 2University of Massachusetts, Worcester, MA; 3UMass, Worcester, MA
Introduction: Dieulafoy lesions are aberrant vessels that cause significant bleeding without ulcers or erosions. They account for about 5% of acute gastrointestinal (GI) hemorrhages. Typically found on the stomach's lesser curvature, these lesions can occur anywhere in the GI tract, with only 2% in the rectum. We present a rare case of a life-threatening rectal Dieulafoy lesion requiring a multidisciplinary approach.
Case Description/Methods: A 73-year-old female with a history of ulcerative colitis, rectal prolapse status post-rectopexy, and coronary artery disease presented after a mechanical fall. The hospital course was complicated by splenic laceration requiring embolization, respiratory failure, fungemia, common femoral artery occlusion requiring thrombectomy, and an abdominal hematoma requiring evacuation. A week into her admission, she developed severe hematochezia becoming tachycardic and hypotensive, necessitating pressors. IV Protonix was started and anticoagulation was held. After resuscitation with blood products, a colonoscopy demonstrated an actively spurting Dieulafoy lesion at the distal rectum 2 cm proximal to the anal verge. Given the location, endoscopic intervention was unable to be performed. Computer Tomography angiogram (CTA) displayed a focal bleed at the inferior rectal artery. Radiology advised against embolization due to its distal location and concerns for causing ischemia. As a result, Colorectal surgery was asked to see the patient. Thrombin-soaked gel foam pads, topical hemostatic agents, and direct pressure were applied initially, followed by direct cauterization to the vessel. Primary hemostasis was achieved and there were no further episodes of rebleeding.
Discussion: Common causes of massive rectal bleeding include hemorrhoids, anal fissures, and fistulas-in-ano, with rectal Dieulafoy lesions being a rare but severe cause. This case highlights the importance of a multidisciplinary approach. Colonoscopy remains the standard for diagnosis and treatment for profuse lower GI bleeding. In this case, direct visualization ruled out other possible causes of lower GI bleed and confirmed an aberrant spurting vessel. Notably, the patient’s post-surgical rectal anatomy, location, and severity of bleeding made endoscopic intervention difficult. When endoscopy and radiologic intervention are limited, surgical evaluation is warranted to intervene. In this case, surgical intervention with manual pressure and mucosal cautery provided definitive hemostasis.
Figure: Figure 1, Figure 2: Images of the spurting rectal bleeding. The culprit lesion was located just above the dentate line and presented as hematochezia. Figure 3: CT angiography of the abdomen and pelvis showing focal extravasation at the inferior rectal artery.
Disclosures:
Rohan Rau indicated no relevant financial relationships.
Sanjay Rau indicated no relevant financial relationships.
Kyle Kreitman indicated no relevant financial relationships.
Rohan Rau, DO1, Sanjay Rau, DO2, Kyle Kreitman, DO3. P2540 - A Life-Threatening Rectal Dieulafoy Lesion Requiring a Multi-Disciplinary Approach, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
