Monday Poster Session
Category: IBD
P2566 - The Longitudinal Cardiovascular Impact of Depression in Patients With IBD: A Large Multi-Center Cohort Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Ethan M. Cohen, MD
West Virginia University
Morgantown, WV
Presenting Author(s)
Ethan M.. Cohen, MD1, Ayowumi A.. Adekolu, MD1, Taylor M.. McCready, MPH2, Justin T.. Kupec, MD1
1West Virginia University, Morgantown, WV; 2NYU Grossman School of Medicine, New York, NY
Introduction: Ulcerative colitis (UC) and Crohn’s disease (CD) are gastrointestinal diseases characterized by immunologically mediated repetitive inflammation of the colon. Recent studies suggest both diseases might increase cardiovascular disease (CVD) risk, but only recently has there been a connection theorized with major depressive disorder (MDD). This study evaluates the CVD risk in UC and CD patients with and without MDD.
Methods: We conducted a population-based, nationwide retrospective cohort study using the TriNetX platform. Adult patients aged ≥18 years old with a confirmed diagnosis of either UC or CD were included. In the intervention group, participants were included if they had a MDD diagnosis at least one month after their initial UC or CD diagnosis. We excluded patients with psychoactive substance-related disorders and a prior cancer diagnosis. Patients who were diagnosed with UC or CD and were diagnosed with MDD at least one month later were matched with patients diagnosed with UC or CD that were never diagnosed with MDD using 1:1 propensity score matching (PSM) according to demographics, essential hypertension, type 1 and type 2 diabetes mellitus, nicotine dependence, and BMI.
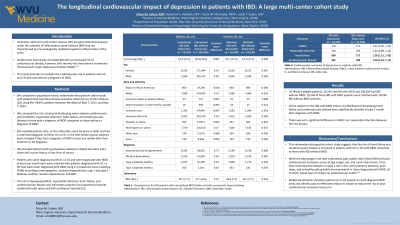
Results: Before PSM, the intervention group with UC or CD and MDD comprised 10,345 patients, while the control group without MDD consisted of 338,269 patients.10,238 patients were matched. If all PSM assumptions hold, we estimate that the lifetime risk of developing heart failure (HF) (OR 1.28; 95%CI 1.15, 1.42) and cerebrovascular disease (OR 1.50; 95%CI 1.32, 1.71) in the intervention arm were significantly increased when compared to the control arm (Table 1). The risks for myocardial infarction and major adverse cardiovascular events were similar in both groups.
Discussion: In this large cohort study, we found that the risk of HF and cerebrovascular disease are increased in patients with UC or CD with MDD compared to those without MDD. While the physiology is not fully understood, past studies have linked MDD and poor cardiovascular outcomes across all age ranges, sex, and rural-urban status. It has been theorized that lifestyle could play a role in this difference, with sedentary behavior, poor sleep, and unhealthy eating habits more prevalent in those diagnosed with MDD, all of which have an impact on cardiovascular health. Given this, deliberate attention should be given to those diagnosed with UC or CD and MDD to reduce the risk of poor cardiovascular outcomes long-term.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ethan M.. Cohen, MD1, Ayowumi A.. Adekolu, MD1, Taylor M.. McCready, MPH2, Justin T.. Kupec, MD1. P2566 - The Longitudinal Cardiovascular Impact of Depression in Patients With IBD: A Large Multi-Center Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1West Virginia University, Morgantown, WV; 2NYU Grossman School of Medicine, New York, NY
Introduction: Ulcerative colitis (UC) and Crohn’s disease (CD) are gastrointestinal diseases characterized by immunologically mediated repetitive inflammation of the colon. Recent studies suggest both diseases might increase cardiovascular disease (CVD) risk, but only recently has there been a connection theorized with major depressive disorder (MDD). This study evaluates the CVD risk in UC and CD patients with and without MDD.
Methods: We conducted a population-based, nationwide retrospective cohort study using the TriNetX platform. Adult patients aged ≥18 years old with a confirmed diagnosis of either UC or CD were included. In the intervention group, participants were included if they had a MDD diagnosis at least one month after their initial UC or CD diagnosis. We excluded patients with psychoactive substance-related disorders and a prior cancer diagnosis. Patients who were diagnosed with UC or CD and were diagnosed with MDD at least one month later were matched with patients diagnosed with UC or CD that were never diagnosed with MDD using 1:1 propensity score matching (PSM) according to demographics, essential hypertension, type 1 and type 2 diabetes mellitus, nicotine dependence, and BMI.
Results: Before PSM, the intervention group with UC or CD and MDD comprised 10,345 patients, while the control group without MDD consisted of 338,269 patients.10,238 patients were matched. If all PSM assumptions hold, we estimate that the lifetime risk of developing heart failure (HF) (OR 1.28; 95%CI 1.15, 1.42) and cerebrovascular disease (OR 1.50; 95%CI 1.32, 1.71) in the intervention arm were significantly increased when compared to the control arm (Table 1). The risks for myocardial infarction and major adverse cardiovascular events were similar in both groups.
Discussion: In this large cohort study, we found that the risk of HF and cerebrovascular disease are increased in patients with UC or CD with MDD compared to those without MDD. While the physiology is not fully understood, past studies have linked MDD and poor cardiovascular outcomes across all age ranges, sex, and rural-urban status. It has been theorized that lifestyle could play a role in this difference, with sedentary behavior, poor sleep, and unhealthy eating habits more prevalent in those diagnosed with MDD, all of which have an impact on cardiovascular health. Given this, deliberate attention should be given to those diagnosed with UC or CD and MDD to reduce the risk of poor cardiovascular outcomes long-term.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ethan Cohen indicated no relevant financial relationships.
Ayowumi Adekolu indicated no relevant financial relationships.
Taylor McCready indicated no relevant financial relationships.
Justin Kupec indicated no relevant financial relationships.
Ethan M.. Cohen, MD1, Ayowumi A.. Adekolu, MD1, Taylor M.. McCready, MPH2, Justin T.. Kupec, MD1. P2566 - The Longitudinal Cardiovascular Impact of Depression in Patients With IBD: A Large Multi-Center Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

