Monday Poster Session
Category: IBD
P2572 - Patterns of Abnormal MUC1 Expression in Patients with Pouchitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jana G. Al Hashash, MD, MSc, FACG
Associate Professor
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Jana G. Hashash, MD, MSc1, Irene Yan, MS1, Raouf Nakhleh, MD1, Michael Camilleri, MD, MACG2, Ahmed Kurdi, MD3, Tushar Patel, MBChB1, William Faubion, MD4, Jonathan Leighton, MD2, Laura E. Raffals, MD2, Francis A. Farraye, MD, MSc1, Fadi F. Francis, MD5
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic, Rochester, MN; 3Mayo Clinic, Rrochester, MN; 4Mayo Clinic, Scottsdale, AZ; 5University of Pittsburgh, Pittsburgh, PA
Introduction: MUC1 glycoprotein is a mucin expressed at low levels and in fully glycosylated form in healthy epithelial cells. Inflammation and cancer result in overexpression and hypoglycosylation of MUC1, which interferes with the protective mucin barrier. Our hypothesis is that overexpression of hypoglycosylated MUC1 is associated with pouchitis severity. Our aim was to investigate MUC1 expression in J-pouch mucosa of patients with varying degrees of pouchitis status post (s/p) ileal pouch anal anastomosis (IPAA) for ulcerative colitis (UC).
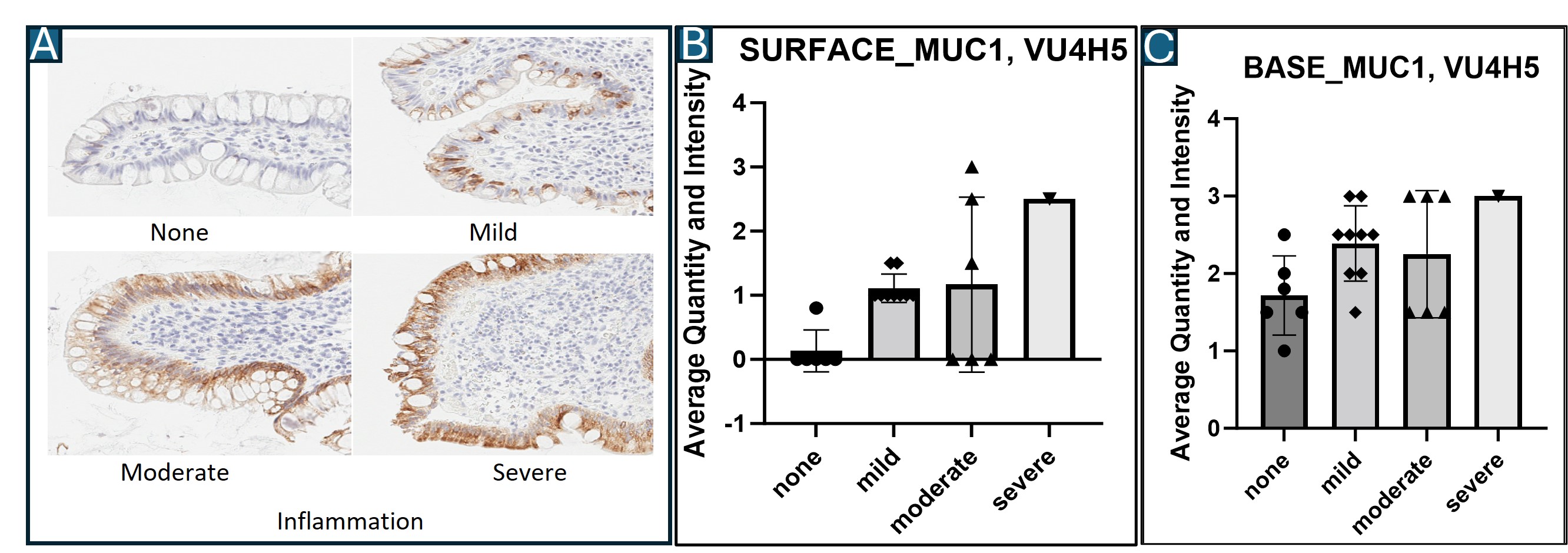
Methods: Archived ileum tissue from the J-pouch of patients with UC s/p IPAA and different degrees of pouchitis (none, mild, moderate or severe) based on histology were identified. Consecutive tissue sections from the ileal J-pouch were stained using two different anti-MUC1 antibodies: HMPV that recognizes all forms of MUC1 and 4H5 that only recognizes abnormal hypoglycosylated MUC1. Each slide was graded based on quantity of staining (score 0-4) and intensity (score 0-4) of MUC1 by a team blinded to the clinical information. The average of these 2 scores was used to calculate a total MUC1 expression score.
Results: Archived tissue from 22 patients with UC/IPAA were obtained: 6 without pouchitis, 9 with mild pouchitis, 6 with moderate pouchitis, and 1 with severe pouchitis. Tissue from patients with no pouchitis showed no expression of the hypoglycosylated/abnormal form of MUC1 on the surface, while tissue from patients with pouchitis demonstrated increasing degrees of expression depending on severity of pouchitis (Figure 1a/1b). Abnormal/hypoglycosylated MUC1 expression at the base of the crypts seemed to be overexpressed in all patients, regardless of presence or degree of pouchitis (Figure 1c).
Discussion: Expression of abnormal MUC1 is absent or minimal on the surface of pouch ileal biopsies of patients with UC and no pouchitis. More severe overexpression of the hypoglycosylated form was found on the surface of ileal biopsies of patients with pouchitis. Thus, MUC1 may serve as an additional biomarker in the identification of patients with more severe pathology and is being investigated as a surrogate for preventing or treating inflammation in patients with pouchitis.
Disclosures:
Jana G. Hashash, MD, MSc1, Irene Yan, MS1, Raouf Nakhleh, MD1, Michael Camilleri, MD, MACG2, Ahmed Kurdi, MD3, Tushar Patel, MBChB1, William Faubion, MD4, Jonathan Leighton, MD2, Laura E. Raffals, MD2, Francis A. Farraye, MD, MSc1, Fadi F. Francis, MD5. P2572 - Patterns of Abnormal MUC1 Expression in Patients with Pouchitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic, Rochester, MN; 3Mayo Clinic, Rrochester, MN; 4Mayo Clinic, Scottsdale, AZ; 5University of Pittsburgh, Pittsburgh, PA
Introduction: MUC1 glycoprotein is a mucin expressed at low levels and in fully glycosylated form in healthy epithelial cells. Inflammation and cancer result in overexpression and hypoglycosylation of MUC1, which interferes with the protective mucin barrier. Our hypothesis is that overexpression of hypoglycosylated MUC1 is associated with pouchitis severity. Our aim was to investigate MUC1 expression in J-pouch mucosa of patients with varying degrees of pouchitis status post (s/p) ileal pouch anal anastomosis (IPAA) for ulcerative colitis (UC).
Methods: Archived ileum tissue from the J-pouch of patients with UC s/p IPAA and different degrees of pouchitis (none, mild, moderate or severe) based on histology were identified. Consecutive tissue sections from the ileal J-pouch were stained using two different anti-MUC1 antibodies: HMPV that recognizes all forms of MUC1 and 4H5 that only recognizes abnormal hypoglycosylated MUC1. Each slide was graded based on quantity of staining (score 0-4) and intensity (score 0-4) of MUC1 by a team blinded to the clinical information. The average of these 2 scores was used to calculate a total MUC1 expression score.
Results: Archived tissue from 22 patients with UC/IPAA were obtained: 6 without pouchitis, 9 with mild pouchitis, 6 with moderate pouchitis, and 1 with severe pouchitis. Tissue from patients with no pouchitis showed no expression of the hypoglycosylated/abnormal form of MUC1 on the surface, while tissue from patients with pouchitis demonstrated increasing degrees of expression depending on severity of pouchitis (Figure 1a/1b). Abnormal/hypoglycosylated MUC1 expression at the base of the crypts seemed to be overexpressed in all patients, regardless of presence or degree of pouchitis (Figure 1c).
Discussion: Expression of abnormal MUC1 is absent or minimal on the surface of pouch ileal biopsies of patients with UC and no pouchitis. More severe overexpression of the hypoglycosylated form was found on the surface of ileal biopsies of patients with pouchitis. Thus, MUC1 may serve as an additional biomarker in the identification of patients with more severe pathology and is being investigated as a surrogate for preventing or treating inflammation in patients with pouchitis.
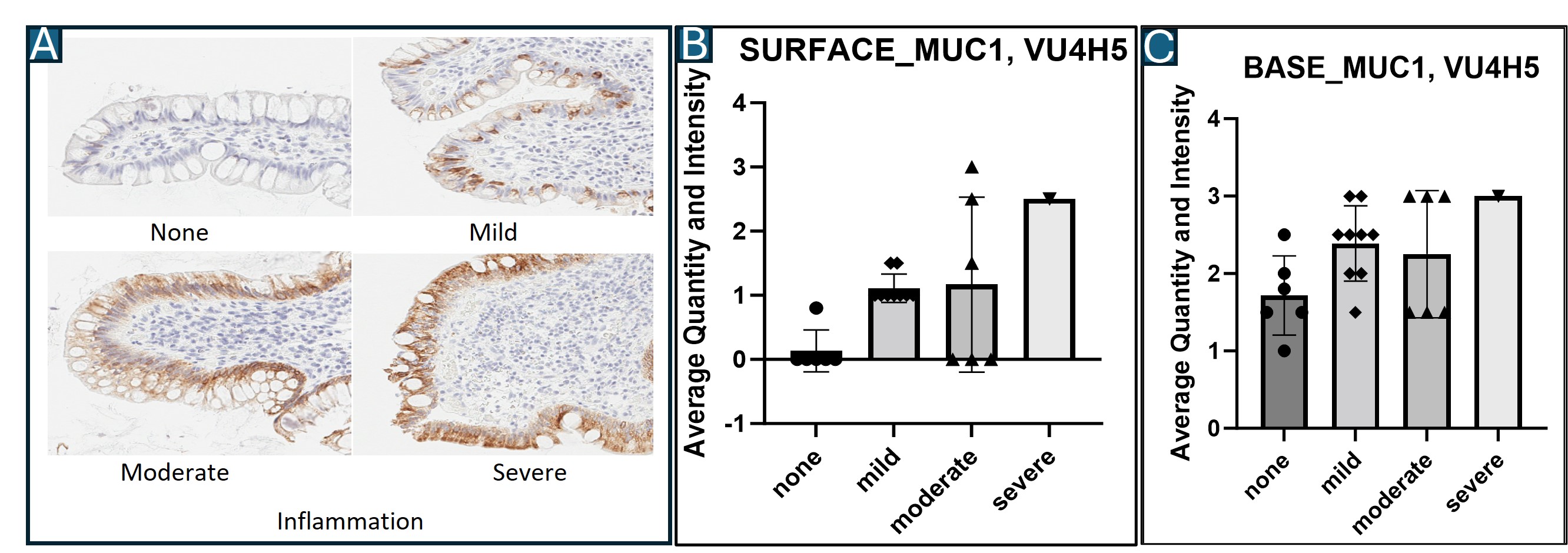
Figure: Figure 1 A/B/C: A. Representative images showing the 4H5 MUC1 stains in ileal J-pouch tissue of patients with different degrees of pouchitis. B. Quantification of abnormal MUC1 expression from the surface of ileal J-pouch tissue of patients with different degrees of pouchitis. C. Quantification of abnormal MUC1 expression from the base of ileal J-pouch tissue of patients with different degrees of pouchitis.
Disclosures:
Jana Hashash: Bristol Myers Squibb – Consultant.
Irene Yan indicated no relevant financial relationships.
Raouf Nakhleh indicated no relevant financial relationships.
Michael Camilleri: Aclipse Therapeutics – Consultant. Aditum Bio – Consultant. Alfasigma – Consultant. APHAIA Pharma – Consultant. Bilayer Therapeutics – Stock Options. Biocodex – Grant/Research Support. BioKier – Consultant. Brightseed Bio – Consultant, Grant/Research Support. Coloplast – Consultant. Cosmo Pharmceuticals – Consultant. Dignify Therapeutics – Stock Options. Enterin – Stock Options. Invea Therapeutics – Consultant. Kallyope – Consultant. Medpace – Consultant. Monteresearch – Consultant. Neurogastrx – Consultant. NGM Biopharmaceuticals – Grant/Research Support. Pfizer – Grant/Research Support. Phenomix – Advisor or Review Panel Member, Stock Options. Renexxion – Consultant. SKYE Bioscience – Consultant. Sumitomo / Sunovion – Consultant. Synlogic – Consultant. Takeda – Consultant. Thelium Therapeutics – Stock Options. Vanda – Grant/Research Support.
Ahmed Kurdi indicated no relevant financial relationships.
Tushar Patel indicated no relevant financial relationships.
William Faubion indicated no relevant financial relationships.
Jonathan Leighton indicated no relevant financial relationships.
Laura E. Raffals: Bristol Myers Squibb – Advisory Committee/Board Member, Consultant. Fresenius Kabi USA – Advisory Committee/Board Member, Consultant. Geneoscopy – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant. Roivant Sciences – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant.
Francis Farraye: AbbVie – Consultant. Avalo Therapeutics – Consultant. Bausch – Advisor or Review Panel Member. BMS – Consultant. Braintree Labs – Consultant. DSMB for Lilly. – Sits on. Fresenius Kabi – Consultant. GI Reviewers and IBD Educational Group – independent contractor. GSK, Iterative Health, Janssen, Pfizer, Pharmacosmos, Sandoz Immunology, Sebela and Viatris – Consultant.
Fadi Francis indicated no relevant financial relationships.
Jana G. Hashash, MD, MSc1, Irene Yan, MS1, Raouf Nakhleh, MD1, Michael Camilleri, MD, MACG2, Ahmed Kurdi, MD3, Tushar Patel, MBChB1, William Faubion, MD4, Jonathan Leighton, MD2, Laura E. Raffals, MD2, Francis A. Farraye, MD, MSc1, Fadi F. Francis, MD5. P2572 - Patterns of Abnormal MUC1 Expression in Patients with Pouchitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
