Monday Poster Session
Category: IBD
P2602 - Development of Anemia and Decreased Ferritin Is Common Among Patients With Ileal Pouch Anal Anastomosis but Is not Associated With Endoscopic Ulcerations of the Pouch
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- ED
Emma F. Dester, MS
Cleveland Clinic Lerner College of Medicine
Cleveland, OH
Presenting Author(s)
Emma F. Dester, MS1, Joseph Carter Powers, BA1, Katherine E. Westbrook, DO2, Mark Zemanek, DO2, Qijun Yang, MS3, Benjamin L. Cohen, MD2, Katherine Falloon, MD4, Suha Abushamma, MD3, Taha Qazi, MD5
1Cleveland Clinic Lerner College of Medicine, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH; 4Cleveland Clinic Foundation, Shaker Heights, OH; 5Cleveland Clinic Foundation, Beachwood, OH
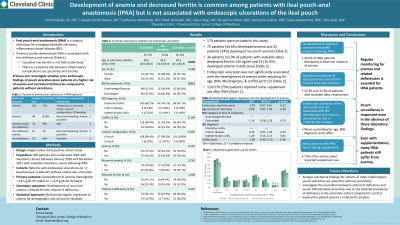
Introduction: Ileal pouch-anal anastomosis (IPAA) is a surgical technique for managing medically refractory inflammatory bowel disease (IBD). Previous studies have demonstrated IPAA is associated with nutritional deficiencies and subsequent anemia. Although the causative mechanism is not fully understood, some studies indicate a link between inflammatory complications (i.e., pouchitis) and anemia. This study aims to investigate whether prior endoscopic findings of pouch ulceration place patients at a higher risk of anemia and nutritional deficiencies compared to patients without ulcerations.
Methods: This is a single-center retrospective cohort study assessing IBD patients who underwent IPAA with ileostomy closure between January 2010 and December 2021 and have available nutritional laboratory values following IPAA. Patients were divided into two groups based on whether endoscopic ulcerations were present on at least one pouchoscopy. The primary outcome was development of anemia (hemoglobin < 13.5 g/dL for males or < 12.0 g/dL for females). Laboratory values including ferritin were also considered. The statistical approach utilized multivariate logistic regression to control for demographic and clinical co-variables.
Results: 170 patients were included in this study, with 102 (60%) having evidence of endoscopic ulceration on at least one pouchoscopy. The cohort with ulcerations was younger at the time of colectomy (median 34.5, IQR 25.2-46.8) compared to the cohort without ulcerations (median 43.0, IQR 32.8-54.0, p = 0.002). There was also a significant difference in BMI, with 39.2% of the endoscopic ulceration group and 60.6% of the control group in the overweight or obese BMI category (p = 0.011). Groups were otherwise similar in terms of demographic and clinical variables. In the entire cohort, 75 patients (44.6%) developed anemia and 25 patients (24.0%) developed recurrent anemia (at least two instances of anemia). Endoscopic ulceration was not significantly associated with the development of anemia while adjusting for age, BMI, IBD diagnosis, and cuffitis (aOR = 1.70, 95% CI 0.87-3.35, p=0.12; Table 1). 36 patients (52.9% of patients with available data) developed ferritin < 45 ng/ml.
Discussion: Development of anemia and decreased ferritin is common among IBD patients following IPAA. Endoscopic ulceration of the ileal pouch is not associated with the development of anemia or decreased ferritin, emphasizing the importance of pouch surveillance even in the absence of these laboratory findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Emma F. Dester, MS1, Joseph Carter Powers, BA1, Katherine E. Westbrook, DO2, Mark Zemanek, DO2, Qijun Yang, MS3, Benjamin L. Cohen, MD2, Katherine Falloon, MD4, Suha Abushamma, MD3, Taha Qazi, MD5. P2602 - Development of Anemia and Decreased Ferritin Is Common Among Patients With Ileal Pouch Anal Anastomosis but Is not Associated With Endoscopic Ulcerations of the Pouch, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Lerner College of Medicine, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH; 4Cleveland Clinic Foundation, Shaker Heights, OH; 5Cleveland Clinic Foundation, Beachwood, OH
Introduction: Ileal pouch-anal anastomosis (IPAA) is a surgical technique for managing medically refractory inflammatory bowel disease (IBD). Previous studies have demonstrated IPAA is associated with nutritional deficiencies and subsequent anemia. Although the causative mechanism is not fully understood, some studies indicate a link between inflammatory complications (i.e., pouchitis) and anemia. This study aims to investigate whether prior endoscopic findings of pouch ulceration place patients at a higher risk of anemia and nutritional deficiencies compared to patients without ulcerations.
Methods: This is a single-center retrospective cohort study assessing IBD patients who underwent IPAA with ileostomy closure between January 2010 and December 2021 and have available nutritional laboratory values following IPAA. Patients were divided into two groups based on whether endoscopic ulcerations were present on at least one pouchoscopy. The primary outcome was development of anemia (hemoglobin < 13.5 g/dL for males or < 12.0 g/dL for females). Laboratory values including ferritin were also considered. The statistical approach utilized multivariate logistic regression to control for demographic and clinical co-variables.
Results: 170 patients were included in this study, with 102 (60%) having evidence of endoscopic ulceration on at least one pouchoscopy. The cohort with ulcerations was younger at the time of colectomy (median 34.5, IQR 25.2-46.8) compared to the cohort without ulcerations (median 43.0, IQR 32.8-54.0, p = 0.002). There was also a significant difference in BMI, with 39.2% of the endoscopic ulceration group and 60.6% of the control group in the overweight or obese BMI category (p = 0.011). Groups were otherwise similar in terms of demographic and clinical variables. In the entire cohort, 75 patients (44.6%) developed anemia and 25 patients (24.0%) developed recurrent anemia (at least two instances of anemia). Endoscopic ulceration was not significantly associated with the development of anemia while adjusting for age, BMI, IBD diagnosis, and cuffitis (aOR = 1.70, 95% CI 0.87-3.35, p=0.12; Table 1). 36 patients (52.9% of patients with available data) developed ferritin < 45 ng/ml.
Discussion: Development of anemia and decreased ferritin is common among IBD patients following IPAA. Endoscopic ulceration of the ileal pouch is not associated with the development of anemia or decreased ferritin, emphasizing the importance of pouch surveillance even in the absence of these laboratory findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Emma Dester indicated no relevant financial relationships.
Joseph Carter Powers: The Crohn's and Colitis Foundation Grant Funding through the Student Research Fellowship Award – Grant/Research Support.
Katherine Westbrook indicated no relevant financial relationships.
Mark Zemanek indicated no relevant financial relationships.
Qijun Yang indicated no relevant financial relationships.
Benjamin L. Cohen: Abbvie – Consultant, support and/or funding, Speakers Bureau. Bristol Myers Squibb – support and/or funding. Celgene – support and/or funding. Emmes – Consultant, Speakers Bureau. Janssen – Consultant, support and/or funding, Speakers Bureau. Pfizer – support and/or funding. Takeda – Consultant, Speakers Bureau. Target RWE – Consultant, Speakers Bureau.
Katherine Falloon: Janssen – Advisory Committee/Board Member. Pfizer – Grant/Research Support.
Suha Abushamma indicated no relevant financial relationships.
Taha Qazi: Abbvie Biosciences – Advisor or Review Panel Member, Consultant, Grant/Research Support, Speakers Bureau. Celgene/BMS – Advisor or Review Panel Member, Speakers Bureau. Janssen – Speakers Bureau. Pfizer – Advisor or Review Panel Member, Advisory Committee/Board Member. Prometheus Biosciences – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant.
Emma F. Dester, MS1, Joseph Carter Powers, BA1, Katherine E. Westbrook, DO2, Mark Zemanek, DO2, Qijun Yang, MS3, Benjamin L. Cohen, MD2, Katherine Falloon, MD4, Suha Abushamma, MD3, Taha Qazi, MD5. P2602 - Development of Anemia and Decreased Ferritin Is Common Among Patients With Ileal Pouch Anal Anastomosis but Is not Associated With Endoscopic Ulcerations of the Pouch, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
