Monday Poster Session
Category: IBD
P2604 - Safety and Effectiveness of Biologic and Small Molecule Therapies in IBD Patients Over the Age of 60
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Neal K. Bhachawat, DO
Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Neal K. Bhachawat, DO1, Shayan Amini, MD2, Wahibah Hannan, BS3, Bincy P. Abraham, MD, MS, FACG4, Christopher Fan, MD5, Kerri Glassner, DO2
1Houston Methodist Hospital, San Antonio, TX; 2Houston Methodist-Weill Cornell Graduate School of Medical Sciences, Houston, TX; 3Texas A&M School of Medicine, Houston, TX; 4Houston Methodist-Weill Cornell, Houston, TX; 5Underwood Center for Digestive Disorders, Houston Methodist Hospital, Houston, TX
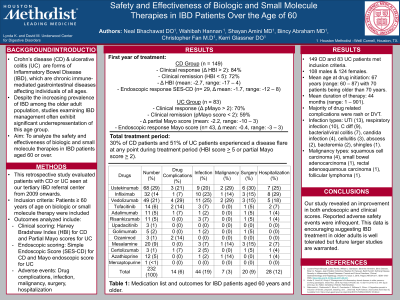
Introduction: Despite the increasing prevalence of inflammatory bowel disease (IBD) among older adults, studies examining its management often exhibit significant underrepresentation of this age group. This study analyzes the safety and effectiveness of biologic and small molecule therapies in IBD patients age > 60 years.
Methods: A retrospective study of patients with Crohn’s disease (CD) and ulcerative colitis (UC), seen at a tertiary IBD referral center from 2009 onwards, age > 60 years treated with biologic and small molecule therapy. Scores collected within one year pre/post therapy initiation included Harvey-Bradshaw Index (HBI), partial Mayo score, Simple Endoscopic Severity-CD (SES-CD) and Mayo scoring. Adverse events included drug complications deemed secondary to therapy, infection, malignancy, surgical intervention and disease related hospitalization.
Results: A total of 232 patients met inclusion criteria (149 CD, 83 UC), 108 males and 124 females. Mean age at drug initiation was 67 years (range:60–87) with seventy patients being > 70 years. Mean duration of therapy was 44 months (range:1–901). Table 1 exhibits study medications and group outcomes. Safety outcomes included: Drug related complication rate of 6% with majority being rash or DVT. Infection rate of 19%: UTI(13), respiratory infection (10), C diff (9), bacterial/viral colitis (7), candida infection (4), cellulitis (3), abscess (2), bacteremia (2), shingles (1). Malignancy rate of 13%: squamous cell carcinoma (4), small bowel adenocarcinoma (1), rectal adenosquamous carcinoma (1), follicular lymphoma (1). In the first year of treatment, 84% of CD and 70% of UC patients achieved clinical response, defined as decrease in the delta HBI or delta pMayo > 2. Additionally, 72% of CD and 59% of UC patients achieved clinical remission defined as an HBI < 5 or pMayo score < 2. Based off the HBI/pMayo score, 30% of CD patients and 51% of UC patients experienced a disease flare during their treatment period. Pre/post therapy initiation revealed an overall decrease in endoscopic score: SES-CD (n=29, delta mean: -1.7,range:-12–8), Mayo score (n=43, delta mean: -0.4,range:-3–3). Post therapy initiation endoscopic remission results: SES-CD score < 3 (n=32) and Mayo score = 0 (n=35).
Discussion: Our study revealed an improvement in both endoscopic and HBI/pMayo scores. Reported safety outcomes as noted above were infrequent. This data is encouraging suggesting IBD treatment in older adults is well tolerated but future larger studies are warranted.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Neal K. Bhachawat, DO1, Shayan Amini, MD2, Wahibah Hannan, BS3, Bincy P. Abraham, MD, MS, FACG4, Christopher Fan, MD5, Kerri Glassner, DO2. P2604 - Safety and Effectiveness of Biologic and Small Molecule Therapies in IBD Patients Over the Age of 60, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Houston Methodist Hospital, San Antonio, TX; 2Houston Methodist-Weill Cornell Graduate School of Medical Sciences, Houston, TX; 3Texas A&M School of Medicine, Houston, TX; 4Houston Methodist-Weill Cornell, Houston, TX; 5Underwood Center for Digestive Disorders, Houston Methodist Hospital, Houston, TX
Introduction: Despite the increasing prevalence of inflammatory bowel disease (IBD) among older adults, studies examining its management often exhibit significant underrepresentation of this age group. This study analyzes the safety and effectiveness of biologic and small molecule therapies in IBD patients age > 60 years.
Methods: A retrospective study of patients with Crohn’s disease (CD) and ulcerative colitis (UC), seen at a tertiary IBD referral center from 2009 onwards, age > 60 years treated with biologic and small molecule therapy. Scores collected within one year pre/post therapy initiation included Harvey-Bradshaw Index (HBI), partial Mayo score, Simple Endoscopic Severity-CD (SES-CD) and Mayo scoring. Adverse events included drug complications deemed secondary to therapy, infection, malignancy, surgical intervention and disease related hospitalization.
Results: A total of 232 patients met inclusion criteria (149 CD, 83 UC), 108 males and 124 females. Mean age at drug initiation was 67 years (range:60–87) with seventy patients being > 70 years. Mean duration of therapy was 44 months (range:1–901). Table 1 exhibits study medications and group outcomes. Safety outcomes included: Drug related complication rate of 6% with majority being rash or DVT. Infection rate of 19%: UTI(13), respiratory infection (10), C diff (9), bacterial/viral colitis (7), candida infection (4), cellulitis (3), abscess (2), bacteremia (2), shingles (1). Malignancy rate of 13%: squamous cell carcinoma (4), small bowel adenocarcinoma (1), rectal adenosquamous carcinoma (1), follicular lymphoma (1). In the first year of treatment, 84% of CD and 70% of UC patients achieved clinical response, defined as decrease in the delta HBI or delta pMayo > 2. Additionally, 72% of CD and 59% of UC patients achieved clinical remission defined as an HBI < 5 or pMayo score < 2. Based off the HBI/pMayo score, 30% of CD patients and 51% of UC patients experienced a disease flare during their treatment period. Pre/post therapy initiation revealed an overall decrease in endoscopic score: SES-CD (n=29, delta mean: -1.7,range:-12–8), Mayo score (n=43, delta mean: -0.4,range:-3–3). Post therapy initiation endoscopic remission results: SES-CD score < 3 (n=32) and Mayo score = 0 (n=35).
Discussion: Our study revealed an improvement in both endoscopic and HBI/pMayo scores. Reported safety outcomes as noted above were infrequent. This data is encouraging suggesting IBD treatment in older adults is well tolerated but future larger studies are warranted.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Neal Bhachawat indicated no relevant financial relationships.
Shayan Amini indicated no relevant financial relationships.
Wahibah Hannan indicated no relevant financial relationships.
Bincy P. Abraham: AbbVie – Consultant, Speakers Bureau. Bristol Myers Squibb – Consultant, Speakers Bureau. Celltrion – Consultant. Eli Lilly – Consultant, Speakers Bureau. Fresenius Kabi – Consultant. Janssen – Consultant, Speakers Bureau. Medtronic – Consultant. Pfizer – Consultant, Speakers Bureau. Prometheus – Consultant. Samsung Bioepis – Consultant. Takeda – Consultant, Speakers Bureau.
Christopher Fan indicated no relevant financial relationships.
Kerri Glassner: Eli Lilly – Advisor or Review Panel Member. Janssen – Advisor or Review Panel Member. Pfizer – Advisor or Review Panel Member, Speakers Bureau.
Neal K. Bhachawat, DO1, Shayan Amini, MD2, Wahibah Hannan, BS3, Bincy P. Abraham, MD, MS, FACG4, Christopher Fan, MD5, Kerri Glassner, DO2. P2604 - Safety and Effectiveness of Biologic and Small Molecule Therapies in IBD Patients Over the Age of 60, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
