Monday Poster Session
Category: IBD
P2607 - Investigating Misdiagnosis Rates of Inflammatory Bowel Disease: A Retrospective Single-Center Review
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Alexander M. Carlson, DO
University at Buffalo
Buffalo, NY
Presenting Author(s)
Alexander M. Carlson, DO1, Courtney Dennis, MD2, Ikjot Singh, MD1, Weam Altaher, DO1, John Cleary, DO1, Himaben Gohil, DO1, Erin Ly, MD1
1University at Buffalo, Buffalo, NY; 2University of Buffalo, Buffalo, NY
Introduction: Accurate diagnosis is critical in the management of inflammatory bowel disease (IBD), yet misdiagnosis remains a significant issue. Carrying a false diagnosis of IBD can lead to numerous adverse effects, including exposure to unnecessary medications, surgical interventions, and the emotional toll of living with a chronic disease. Patients with an incorrect IBD diagnosis may experience avoidable side effects from treatments, increased healthcare costs, and reduced quality of life. This single-center study aims to retrospectively analyze the prevalence of false IBD diagnoses and highlight the importance of accurate diagnostic practices to prevent these detrimental outcomes.
Methods: At a large hospital, we identified 265 patients with a diagnosis of either Crohn’s disease or ulcerative colitis who were seen at our gastroenterology clinic from 2020 to 2023. The patient’s charts were accessed using a local electronic medical record and were cross referenced with a regional electronic medical record for Western New York. To assess for a definitive diagnosis of either Crohn’s disease or ulcerative colitis, the results of endoscopic and pathology reports were recorded.
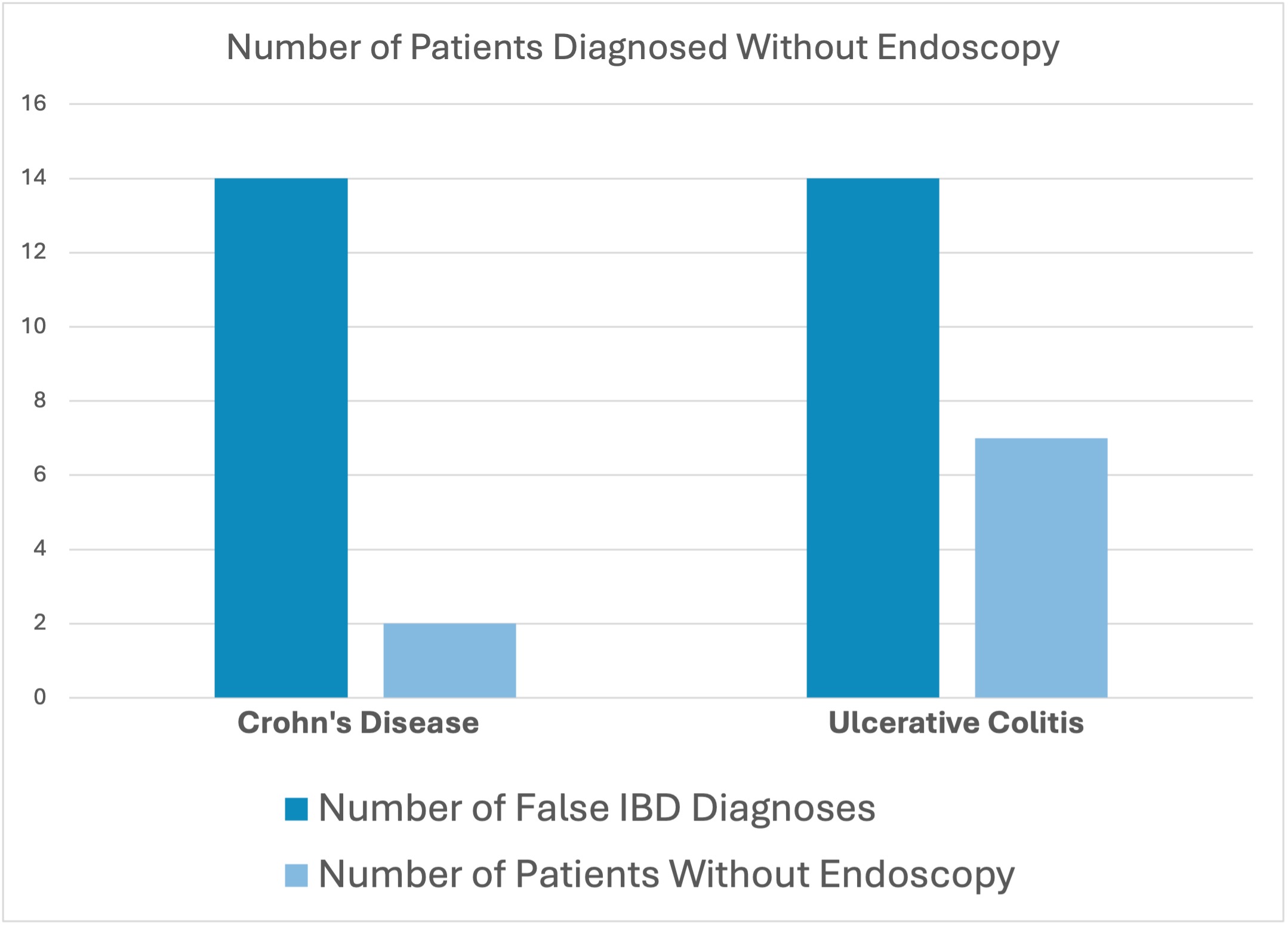
Results: Of the 265 patients analyzed, there were 28 patients (10.6%) with a diagnosis of IBD that could not be confirmed through endoscopy, pathology, or medication fill history. Interestingly, 14 patients (5.3%) carried a diagnosis of ulcerative colitis and 14 patients (5.3%) had a diagnosis of Crohn’s disease. The average patient age was 47. For 19 of these patients, their diagnosis of IBD was ruled out due to negative serum inflammatory markers, lack of symptoms, with normal current and prior endoscopies. 9 patients carried a diagnosis without ever receiving endoscopy (Figure 1).
Discussion: The prevalence of misdiagnosed or misreported IBD highlights the importance of astute medical documentation and diagnosis. The financial strain of managing a misdiagnosed condition, coupled with the psychological toll of navigating a healthcare system, underscores the importance of improving diagnostic precision. By enhancing diagnostic approaches and promoting interdisciplinary collaboration, healthcare providers can mitigate the adverse impacts of misdiagnosis and optimize patient care outcomes in suspected cases of IBD.
Disclosures:
Alexander M. Carlson, DO1, Courtney Dennis, MD2, Ikjot Singh, MD1, Weam Altaher, DO1, John Cleary, DO1, Himaben Gohil, DO1, Erin Ly, MD1. P2607 - Investigating Misdiagnosis Rates of Inflammatory Bowel Disease: A Retrospective Single-Center Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2University of Buffalo, Buffalo, NY
Introduction: Accurate diagnosis is critical in the management of inflammatory bowel disease (IBD), yet misdiagnosis remains a significant issue. Carrying a false diagnosis of IBD can lead to numerous adverse effects, including exposure to unnecessary medications, surgical interventions, and the emotional toll of living with a chronic disease. Patients with an incorrect IBD diagnosis may experience avoidable side effects from treatments, increased healthcare costs, and reduced quality of life. This single-center study aims to retrospectively analyze the prevalence of false IBD diagnoses and highlight the importance of accurate diagnostic practices to prevent these detrimental outcomes.
Methods: At a large hospital, we identified 265 patients with a diagnosis of either Crohn’s disease or ulcerative colitis who were seen at our gastroenterology clinic from 2020 to 2023. The patient’s charts were accessed using a local electronic medical record and were cross referenced with a regional electronic medical record for Western New York. To assess for a definitive diagnosis of either Crohn’s disease or ulcerative colitis, the results of endoscopic and pathology reports were recorded.
Results: Of the 265 patients analyzed, there were 28 patients (10.6%) with a diagnosis of IBD that could not be confirmed through endoscopy, pathology, or medication fill history. Interestingly, 14 patients (5.3%) carried a diagnosis of ulcerative colitis and 14 patients (5.3%) had a diagnosis of Crohn’s disease. The average patient age was 47. For 19 of these patients, their diagnosis of IBD was ruled out due to negative serum inflammatory markers, lack of symptoms, with normal current and prior endoscopies. 9 patients carried a diagnosis without ever receiving endoscopy (Figure 1).
Discussion: The prevalence of misdiagnosed or misreported IBD highlights the importance of astute medical documentation and diagnosis. The financial strain of managing a misdiagnosed condition, coupled with the psychological toll of navigating a healthcare system, underscores the importance of improving diagnostic precision. By enhancing diagnostic approaches and promoting interdisciplinary collaboration, healthcare providers can mitigate the adverse impacts of misdiagnosis and optimize patient care outcomes in suspected cases of IBD.
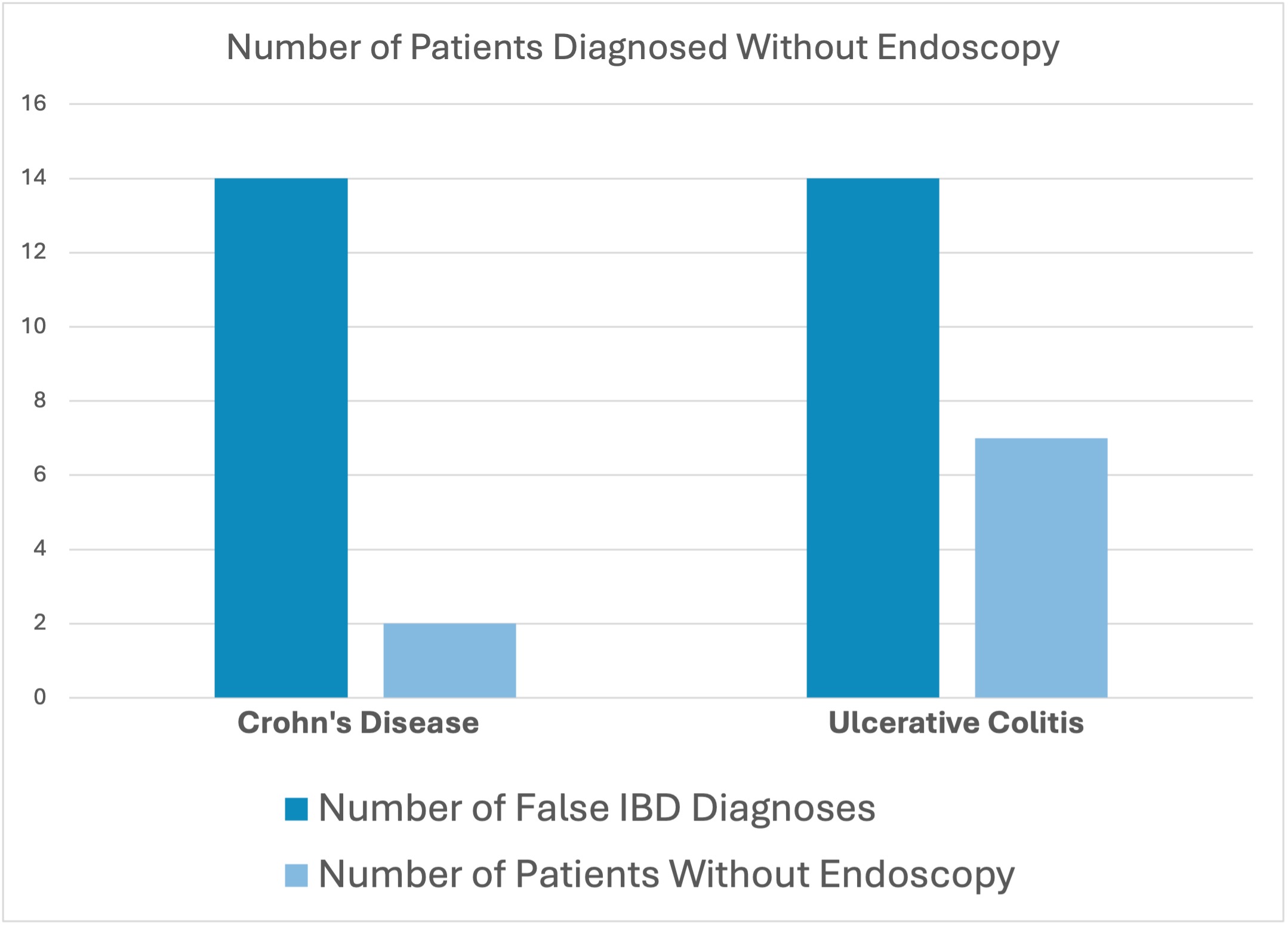
Figure: Figure 1: Bar graph representing the total number of patients who carried a diagnosis of UC or CD and the number of patients in each group who had never underwent endoscopy.
Disclosures:
Alexander Carlson indicated no relevant financial relationships.
Courtney Dennis indicated no relevant financial relationships.
Ikjot Singh indicated no relevant financial relationships.
Weam Altaher indicated no relevant financial relationships.
John Cleary indicated no relevant financial relationships.
Himaben Gohil indicated no relevant financial relationships.
Erin Ly indicated no relevant financial relationships.
Alexander M. Carlson, DO1, Courtney Dennis, MD2, Ikjot Singh, MD1, Weam Altaher, DO1, John Cleary, DO1, Himaben Gohil, DO1, Erin Ly, MD1. P2607 - Investigating Misdiagnosis Rates of Inflammatory Bowel Disease: A Retrospective Single-Center Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
