Monday Poster Session
Category: IBD
P2633 - Impact of Mild Endoscopic Disease Activity on Short-Term Clinical Outcomes in Older Adults With Inflammatory Bowel Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Catherine Z. Tang, BA
NYU Grossman School of Medicine
New York, NY
Presenting Author(s)
Award: Presidential Poster Award
Catherine Z.. Tang, BA1, Olivia R. Delau, MS2, Seymour Katz, MD3, Jordan Axelrad, MD, MPH1, Aasma Shaukat, MD, MPH4, Adam S.. Faye, MD1
1NYU Grossman School of Medicine, New York, NY; 2NYU Langone Health Inflammatory Bowel Disease Center, Cortlandt Manor, NY; 3NYU Grossman School of Medicine, New Hyde Park, NY; 4NYU Langone Health, New York, NY
Introduction: In older adults with inflammatory bowel disease (IBD), the benefits of achieving endoscopic remission among those with mild persistent disease activity are unknown. We aimed to determine whether older adults with mild ongoing endoscopic disease activity had an increased risk of adverse outcomes as compared to those in endoscopic remission.
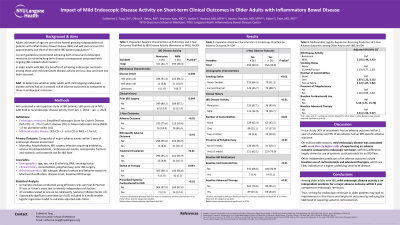
Methods: We conducted a retrospective study of adults ≥ 60 years old with IBD from Jan. 1, 2018 - Jan. 1, 2023. Endoscopic remission was defined as Simplified Endoscopic Score for Crohn’s Disease (SES-CD) = 0 - 2 for Crohn’s disease (CD) or Mayo Endoscopic Score (MES) = 0 for ulcerative colitis (UC). Mild endoscopic disease was defined as SES-CD = 3 - 6 for CD or MES = 1 for UC. The primary outcome was a composite of major adverse events (mortality, hospitalization, IBD surgery, infection, venous thromboembolism, cardiovascular events, osteoporotic fracture, and systemic corticosteroid use for IBD flare) within 1 year of endoscopic assessment. We performed univariate and multivariate analyses, reporting adjusted odds ratios (aORs) with 95% confidence intervals (CIs).
Results: Of the 279 patients who met inclusion criteria (126 with CD, 150 with UC, and 3 with indeterminate colitis), 109 (39.1%) had mild endoscopic disease whereas 170 (60.9%) were in endoscopic remission. At the time of endoscopy, 53.4% of patients were on mesalamine and 36.6% of patients were on an advanced therapy. Within 1 year of endoscopy, treatment was escalated in 15.6% of individuals with mild disease activity vs. 7.1% of those initially in endoscopic remission (p = 0.02). Patients with mild disease activity were also at higher risk of an adverse outcome compared to those in endoscopic remission (42.2% vs. 25.3%, p < 0.01), which was largely driven by use of systemic corticosteroids for a new IBD flare (12.8% vs. 2.4%, p < 0.01). While adjusting for smoking status, number of comorbidities, polypharmacy, baseline corticosteroid use, mesalamine use, and advanced therapy use, mild endoscopic disease was associated with a more than two-fold higher risk of an adverse outcome at 1 year (aOR 2.36, 95% CI 1.35 - 4.12).
Discussion: Among older adults with IBD, mild endoscopic disease activity is an independent predictor for an adverse outcome within 1 year compared to endoscopic remission. Thus, striving for endoscopic remission in older patients may lead to improvement in short-term and long-term outcomes by reducing the likelihood of requiring systemic corticosteroids.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Catherine Z.. Tang, BA1, Olivia R. Delau, MS2, Seymour Katz, MD3, Jordan Axelrad, MD, MPH1, Aasma Shaukat, MD, MPH4, Adam S.. Faye, MD1. P2633 - Impact of Mild Endoscopic Disease Activity on Short-Term Clinical Outcomes in Older Adults With Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Catherine Z.. Tang, BA1, Olivia R. Delau, MS2, Seymour Katz, MD3, Jordan Axelrad, MD, MPH1, Aasma Shaukat, MD, MPH4, Adam S.. Faye, MD1
1NYU Grossman School of Medicine, New York, NY; 2NYU Langone Health Inflammatory Bowel Disease Center, Cortlandt Manor, NY; 3NYU Grossman School of Medicine, New Hyde Park, NY; 4NYU Langone Health, New York, NY
Introduction: In older adults with inflammatory bowel disease (IBD), the benefits of achieving endoscopic remission among those with mild persistent disease activity are unknown. We aimed to determine whether older adults with mild ongoing endoscopic disease activity had an increased risk of adverse outcomes as compared to those in endoscopic remission.
Methods: We conducted a retrospective study of adults ≥ 60 years old with IBD from Jan. 1, 2018 - Jan. 1, 2023. Endoscopic remission was defined as Simplified Endoscopic Score for Crohn’s Disease (SES-CD) = 0 - 2 for Crohn’s disease (CD) or Mayo Endoscopic Score (MES) = 0 for ulcerative colitis (UC). Mild endoscopic disease was defined as SES-CD = 3 - 6 for CD or MES = 1 for UC. The primary outcome was a composite of major adverse events (mortality, hospitalization, IBD surgery, infection, venous thromboembolism, cardiovascular events, osteoporotic fracture, and systemic corticosteroid use for IBD flare) within 1 year of endoscopic assessment. We performed univariate and multivariate analyses, reporting adjusted odds ratios (aORs) with 95% confidence intervals (CIs).
Results: Of the 279 patients who met inclusion criteria (126 with CD, 150 with UC, and 3 with indeterminate colitis), 109 (39.1%) had mild endoscopic disease whereas 170 (60.9%) were in endoscopic remission. At the time of endoscopy, 53.4% of patients were on mesalamine and 36.6% of patients were on an advanced therapy. Within 1 year of endoscopy, treatment was escalated in 15.6% of individuals with mild disease activity vs. 7.1% of those initially in endoscopic remission (p = 0.02). Patients with mild disease activity were also at higher risk of an adverse outcome compared to those in endoscopic remission (42.2% vs. 25.3%, p < 0.01), which was largely driven by use of systemic corticosteroids for a new IBD flare (12.8% vs. 2.4%, p < 0.01). While adjusting for smoking status, number of comorbidities, polypharmacy, baseline corticosteroid use, mesalamine use, and advanced therapy use, mild endoscopic disease was associated with a more than two-fold higher risk of an adverse outcome at 1 year (aOR 2.36, 95% CI 1.35 - 4.12).
Discussion: Among older adults with IBD, mild endoscopic disease activity is an independent predictor for an adverse outcome within 1 year compared to endoscopic remission. Thus, striving for endoscopic remission in older patients may lead to improvement in short-term and long-term outcomes by reducing the likelihood of requiring systemic corticosteroids.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Catherine Tang indicated no relevant financial relationships.
Olivia Delau indicated no relevant financial relationships.
Seymour Katz indicated no relevant financial relationships.
Jordan Axelrad: Abbvie – Consultant. Adiso – Consultant. Biomerieux – Consultant. BMS – Consultant. Fresenius – Consultant. Genentech – Grant/Research Support. Janssen – Consultant. Pfizer – Consultant.
Aasma Shaukat: iterative health; Freenome – Consultant.
Adam Faye: Abbvie – Consultant. BMS – Consultant. Takeda – Education Seminar.
Catherine Z.. Tang, BA1, Olivia R. Delau, MS2, Seymour Katz, MD3, Jordan Axelrad, MD, MPH1, Aasma Shaukat, MD, MPH4, Adam S.. Faye, MD1. P2633 - Impact of Mild Endoscopic Disease Activity on Short-Term Clinical Outcomes in Older Adults With Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

