Monday Poster Session
Category: IBD
P2675 - Association of Faecal Calprotectin With Symptomatic, Endoscopic, and Clinical Remission in Patients With Moderately to Severely Active Ulcerative Colitis Treated With Mirikizumab
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Millie D. Long, MD, MPH
Center for Gastrointestinal Biology and Disease, University of North Carolina
Chapel Hill, NC
Presenting Author(s)
Séverine Vermeire, MD, PhD1, Millie D. Long, MD, MPH2, Parambir S. Dulai, MD3, Christopher Ma, MD4, Faye Chan-diehl, 5, Richard Moses, 5, Baojin Zhu, 5, Jerome Paulissen, 6, Simon Travis, 7, Remo Panaccione, MD4
1University Hospitals Leuven, Leuven, Vlaams-Brabant, Belgium; 2Center for Gastrointestinal Biology and Disease, University of North Carolina, Chapel Hill, NC; 3Feinberg School of Medicine, Northwestern University, Chicago, IL; 4University of Calgary, Calgary, AB, Canada; 5Eli Lilly and Company, Indianapolis, IN; 6Syneos Health, Morrisville, NC; 7University of Oxford, Oxford, England, United Kingdom
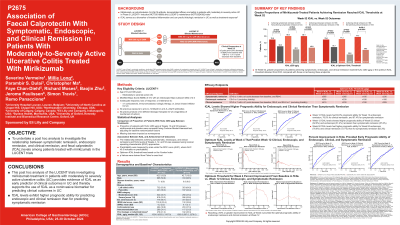
Introduction: Mirikizumab (miri), a p19-directed IL-23 antibody, has been shown to be effective in patients with moderately-to-severely active ulcerative colitis (UC) in Phase 3 trials (LUCENT-1 NCT03518086; LUCENT-2 NCT03524092). The relationship between symptomatic, endoscopic, and clinical remission and levels of the inflammatory biomarker faecal calprotectin (fCAL) was studied for miri-treated patients enrolled in the trials.
Methods: This post hoc analysis evaluated patients treated with intravenous (IV) miri 300mg every 4 weeks (Q4W) until week (W)12 in induction (n=868) followed by subcutaneous miri (n=365) Q4W up to W52 (miri induction responders at W12 who were rerandomized for the maintenance period) or placebo. The improvement in fCAL at W12 and W52 between miri and placebo were compared using Cochran Mantel Haenszel, adjusting for randomization stratification factors. Missing data were imputed as nonresponse. The relationship between achieving symptomatic, endoscopic, or clinical remission (defined in Table) and fCAL levels at W4, W12 and W52 was assessed using receiver operating characteristic (ROC) approaches. Predictability was measured by area under the ROC curve (AUC), and AUC≤0.5 indicates no predictability. Optimal fCAL threshold was obtained based on Youden Index.
Results: Greater proportions of miri-treated patients compared to placebo achieved fCAL≤250 ug/g at W4, W12, and W52. A total of 19.0% vs. 12.5%, 34.3% vs. 20.1%, 50.7% vs 19.3% patients achieved fCAL≤250 ug/g at W4, W12, and W52 miri vs. placebo, respectively. Greater proportions of patients achieving symptomatic, endoscopic, and clinical remission reached the predefined threshold of fCAL≤250 ug/g or the optimum fCAL threshold obtained from the ROC (see Table footnote) in this study compared with those not achieving the endpoints (Table). W4 fCAL levels had 70.5% predictability for W12 endoscopic remission and 64.9% for clinical remission, but lower predictability for symptomatic remission (59.1%). W12 fCAL levels had 83.0% predictability for W12 endoscopic remission, 78.5% for clinical remission, and 67.4% for symptomatic remission. W52 fCAL levels had higher predictability for W52 endoscopic (76.6%) and clinical remission (72.7%) than for symptomatic remission (62.3%).
Discussion: These results support the use of fCAL as an early predictor of clinical outcomes and as a non-invasive biomarker for predicting clinical outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Séverine Vermeire, MD, PhD1, Millie D. Long, MD, MPH2, Parambir S. Dulai, MD3, Christopher Ma, MD4, Faye Chan-diehl, 5, Richard Moses, 5, Baojin Zhu, 5, Jerome Paulissen, 6, Simon Travis, 7, Remo Panaccione, MD4. P2675 - Association of Faecal Calprotectin With Symptomatic, Endoscopic, and Clinical Remission in Patients With Moderately to Severely Active Ulcerative Colitis Treated With Mirikizumab, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University Hospitals Leuven, Leuven, Vlaams-Brabant, Belgium; 2Center for Gastrointestinal Biology and Disease, University of North Carolina, Chapel Hill, NC; 3Feinberg School of Medicine, Northwestern University, Chicago, IL; 4University of Calgary, Calgary, AB, Canada; 5Eli Lilly and Company, Indianapolis, IN; 6Syneos Health, Morrisville, NC; 7University of Oxford, Oxford, England, United Kingdom
Introduction: Mirikizumab (miri), a p19-directed IL-23 antibody, has been shown to be effective in patients with moderately-to-severely active ulcerative colitis (UC) in Phase 3 trials (LUCENT-1 NCT03518086; LUCENT-2 NCT03524092). The relationship between symptomatic, endoscopic, and clinical remission and levels of the inflammatory biomarker faecal calprotectin (fCAL) was studied for miri-treated patients enrolled in the trials.
Methods: This post hoc analysis evaluated patients treated with intravenous (IV) miri 300mg every 4 weeks (Q4W) until week (W)12 in induction (n=868) followed by subcutaneous miri (n=365) Q4W up to W52 (miri induction responders at W12 who were rerandomized for the maintenance period) or placebo. The improvement in fCAL at W12 and W52 between miri and placebo were compared using Cochran Mantel Haenszel, adjusting for randomization stratification factors. Missing data were imputed as nonresponse. The relationship between achieving symptomatic, endoscopic, or clinical remission (defined in Table) and fCAL levels at W4, W12 and W52 was assessed using receiver operating characteristic (ROC) approaches. Predictability was measured by area under the ROC curve (AUC), and AUC≤0.5 indicates no predictability. Optimal fCAL threshold was obtained based on Youden Index.
Results: Greater proportions of miri-treated patients compared to placebo achieved fCAL≤250 ug/g at W4, W12, and W52. A total of 19.0% vs. 12.5%, 34.3% vs. 20.1%, 50.7% vs 19.3% patients achieved fCAL≤250 ug/g at W4, W12, and W52 miri vs. placebo, respectively. Greater proportions of patients achieving symptomatic, endoscopic, and clinical remission reached the predefined threshold of fCAL≤250 ug/g or the optimum fCAL threshold obtained from the ROC (see Table footnote) in this study compared with those not achieving the endpoints (Table). W4 fCAL levels had 70.5% predictability for W12 endoscopic remission and 64.9% for clinical remission, but lower predictability for symptomatic remission (59.1%). W12 fCAL levels had 83.0% predictability for W12 endoscopic remission, 78.5% for clinical remission, and 67.4% for symptomatic remission. W52 fCAL levels had higher predictability for W52 endoscopic (76.6%) and clinical remission (72.7%) than for symptomatic remission (62.3%).
Discussion: These results support the use of fCAL as an early predictor of clinical outcomes and as a non-invasive biomarker for predicting clinical outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Séverine Vermeire: AbbVie – Consultant, Grant/Research Support. Abivax – Consultant. AbolerlsPharma – Consultant. AgomAb – Consultant. Alimentiv – Consultant. Arena Pharmaceuticals – Consultant. AstraZeneca – Consultant. BioraTherapeutics – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant. Celgene – Consultant. Cytoki Pharma – Consultant. Dr Falk Pharma – Consultant. Eli Lilly – Consultant. Ferring – Consultant. Galapagos – Consultant, Grant/Research Support. Genentech Roche – Consultant. Gilead – Consultant. GSK – Consultant. Hospira – Consultant. J&J – Consultant, Grant/Research Support. Janssen – Consultant. lmidomics – Consultant. Materia Prima – Consultant. Mestag Therapeutics – Consultant. Microbiotica – Consultant. MiroBio – Consultant. Morphic – Consultant. MrMHealth – Consultant. MSD – Consultant. Mundipharma – Consultant. Pfizer Inc – Consultant, Grant/Research Support. Prodigest – Consultant. Progenity – Consultant. Prometheus – Consultant. Robarts Clinical Trials – Consultant. Surrozen – Consultant. Takeda – Consultant, Grant/Research Support. Theravance – Consultant. Tillots Pharma AG – Consultant. VectivBio – Consultant. Ventyx – Consultant. Zealand Pharma – Consultant.
Millie Long: AbbVie – Consultant. Bristol-Myers Squibb – Consultant. Eli Lilly – Consultant, Grant/Research Support. Intercept – Consultant. Janssen – Consultant. Pfizer Inc – Consultant, Grant/Research Support. Prometheus – Consultant. Roche – Consultant. Roivant – Consultant. Takeda – Consultant, Grant/Research Support. Target RWE – Consultant.
Parambir Dulai: AbbVie – Consultant. Abivax – Consultant. Adiso – Consultant. Bristol Meyer Squibb – Consultant. Digbi Health – Royalties. Digbi Health – Stock Options. Geneoscopy – Consultant. GSK – Consultant. Janssen – Consultant. Lilly – Consultant. Pfizer – Consultant, Grant/Research Support. Precidiag – Licensing royalties. Takeda – Consultant, Grant/Research Support.
Christopher Ma: AbbVie – Consultant, Speakers Bureau. Alimentiv (formerly Robarts Clinical Trials Inc.) – Consultant, Speakers Bureau. Amgen – Consultant, Speakers Bureau. AVIR Pharma Inc – Consultant, Speakers Bureau. BioJAMP – Consultant. Bristol Myers Squibb – Consultant, Speakers Bureau. Celltrion – Consulting Fees. Ferring – Consultant, Grant/Research Support, Speakers Bureau. Fresenius Kabi – Consultant, Speakers Bureau. Janssen – Consultant, Speakers Bureau. McKesson – Consultant. Mylan – Consultant. Pendopharm – Consultant, Speakers Bureau. Pfizer – Consultant, Grant/Research Support, Speakers Bureau. Prometheus Biosciences Inc. – Consulting Fees. Roche – Consultant. Sanofi – Speaker Fee. Takeda – Consultant, Speakers Bureau.
Faye Chan-diehl: Eli Lilly and Company – Employee, Stock Options.
Richard Moses: Eli Lilly and Company – Employee, Stock Options.
Baojin Zhu: Eli Lilly and Company – Employee, Stock Options.
Jerome Paulissen: Syneos Health – Employee.
Simon Travis: AbbVie – Grant/Research Support. Buhlmann – Grant/Research Support. ECCO – Grant/Research Support. Eli Lilly and Company – Grant/Research Support. Ferring Pharmaceuticals – Grant/Research Support. International Organization for the Study of IBD – Grant/Research Support. Janssen – Grant/Research Support. MSD – Grant/Research Support. Normal Collision Foundation – Grant/Research Support. Pfizer – Grant/Research Support. Procter & Gamble – Grant/Research Support. Schering-Plough – Grant/Research Support. Takeda – Grant/Research Support. UCB – Grant/Research Support. Vifor Pharma – Grant/Research Support. Warner Chilcott – Grant/Research Support.
Remo Panaccione: Élan – Consultant. Abbivax – Consultant. Abbott – Consultant. AbbVie – Advisory Committee/Board Member, Consultant, Speaking Fees. Alimentiv – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member, Consultant, Speaker Fees. Arena Pharmaceuticals – Advisory Committee/Board Member, Consultant, Speaker Fees. AstraZeneca – Advisory Committee/Board Member, Consultant. Biogen – Advisory Committee/Board Member, Consultant. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speaker Fees. Celgene – Advisory Committee/Board Member, Consultant, Speaker Fees. Celltrion – Consultant. Cosmos Pharmaceuticals – Consultant. Eisai – Consultant. Ferring – Advisory Committee/Board Member, Consultant, Speaker Fees. Fresenius Kabi – Advisory Committee/Board Member, Consultant, Speaker Fees. Galapagos – Consultant. Genentech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant, Speaker Fees. GlaxoSmithKline – Advisory Committee/Board Member, Consultant. JAMP Bio – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant, Speaker Fees. Lilly – Advisory Committee/Board Member, Consultant, Speaker Fees. Merck – Advisory Committee/Board Member, Consultant, Speaker Fees. Mylan – Advisory Committee/Board Member, Consultant. Novartis – Advisory Committee/Board Member, Consultant. Oppilan Pharma – Advisory Committee/Board Member, Consultant. Organon – Advisory Committee/Board Member, Consultant, Speaker Fees. Pandion Pharma – Advisory Committee/Board Member, Consultant. Pendopharm – Consultant. Pfizer Inc – Advisory Committee/Board Member, Consultant, Speaker Fees. Progenity – Advisory Committee/Board Member, Consultant. Prometheus Biosciences – Consultant. Protagonist Therapeutics – Advisory Committee/Board Member, Consultant. Roche – Advisory Committee/Board Member, Consultant, Speaker Fees. Sandoz – Advisory Committee/Board Member, Consultant, Speaker Fees. Satisfai Health – Consultant. Shire – Advisory Committee/Board Member, Consultant, Speaker Fees. Sublimity Therapeutics – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Speaker Fees. Theravance – Consultant. Trellus – Consultant. UCB – Consultant. Ventyx – Advisory Committee/Board Member, Consultant. Viatris – Consultant.
Séverine Vermeire, MD, PhD1, Millie D. Long, MD, MPH2, Parambir S. Dulai, MD3, Christopher Ma, MD4, Faye Chan-diehl, 5, Richard Moses, 5, Baojin Zhu, 5, Jerome Paulissen, 6, Simon Travis, 7, Remo Panaccione, MD4. P2675 - Association of Faecal Calprotectin With Symptomatic, Endoscopic, and Clinical Remission in Patients With Moderately to Severely Active Ulcerative Colitis Treated With Mirikizumab, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
