Monday Poster Session
Category: IBD
P2678 - Mapping Culturable Microbes of Perianal Fistula in Patients With Crohn’s Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Felix D. Rozenberg, MD
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Felix D. Rozenberg, MD1, Samuel Pan, MD2, Joshua Lacoste, BA2, Elisabeth Giselbrecht, 2, Serre-yu Wong, MD, PhD2
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Perianal fistulizing Crohn’s disease (PFCD) is a severe manifestation of Crohn’s disease (CD). The fistula microbiome has been shown to be unique in patients with PFCD. However, the role of individual microbes in fistula pathogenesis remains unexplored. To describe and obtain bacterial species of fistula tracts for mechanistic studies, we aim to establish broad culture of bacteria from perianal fistulas and evaluate changes in the fistula microbiome relative to disease outcomes.
Methods: We conducted a prospective observational study of 80 adult patients with perianal disease undergoing exam under anesthesia (EUA). During EUA, specimens were collected from three sites of the fistula tunnels: (1) swab of perianal skin surrounding the external opening, (2) brushing of fistula tract, and (3) brushing of the inner opening in the rectum. Samples from two patients with both freshly collected and frozen samples were compared. Samples were plated and grown in anaerobic, microaerophilic, and aerobic conditions. Individual colonies were picked for strain identification by MALDI-TOF.
Results: Of the 80 patients, 62 (77.5%) had PFCD, 7 (8.8%) had ileal pouch-anal anastomosis fistulas, and 11 (13.8%) were non-IBD controls. We further collected longitudinal samples from 10 adults with PFCD and one with a non-CD fistula. Table 1 describes the disease progression of these patients between sample collection dates.
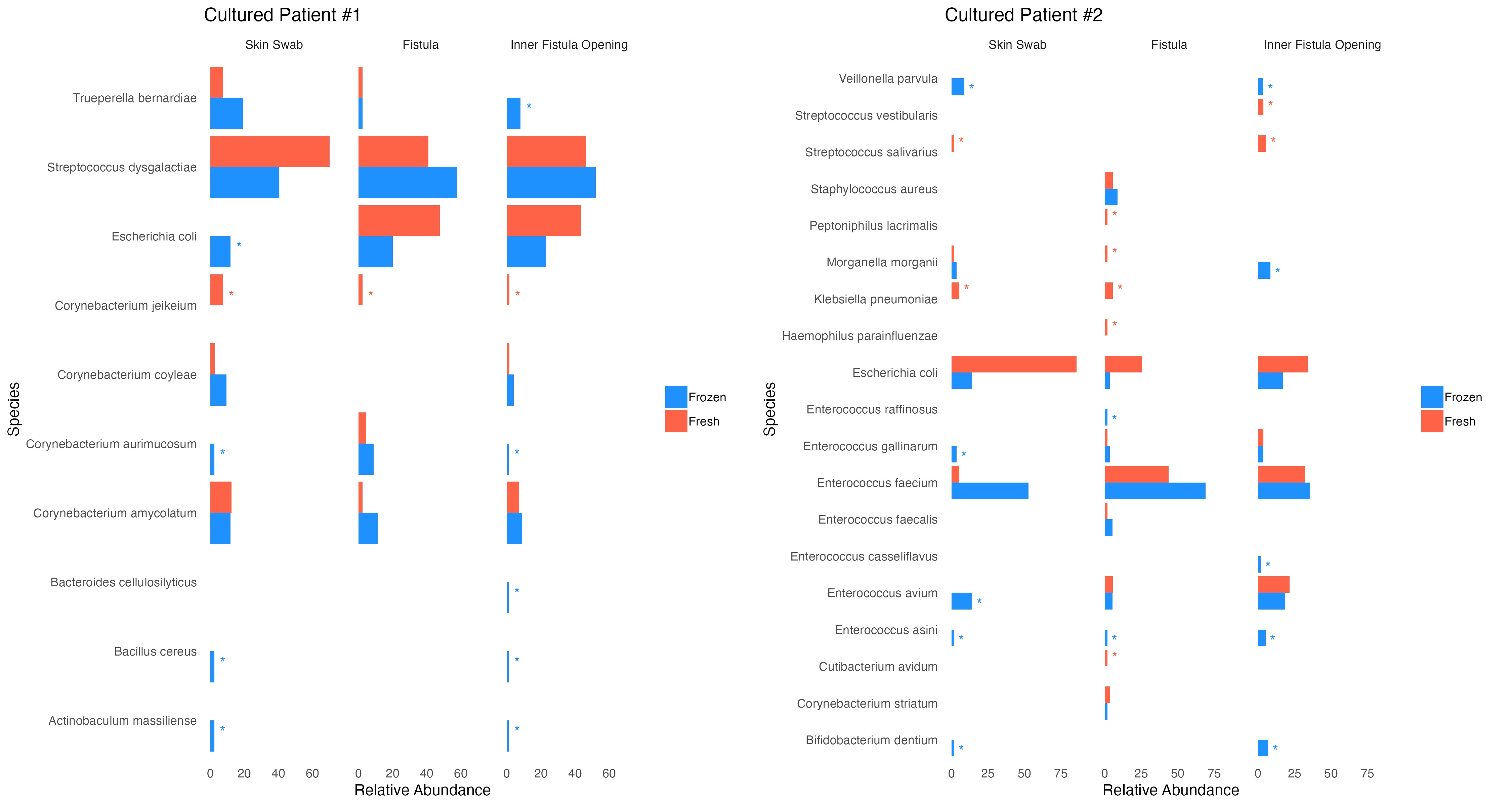
Here, we show data from culturing specimens from two patients. The bacterial strains cultured from within the fistula were a mix of intestinal and skin-colonizing bacteria (Figure 1). Similar strains were cultured from both fresh and frozen specimens. Multiple bacterial strains commonly known to colonize skin were cultured from both the internal and external fistula opening brushings, such as S. aureus, S. dysgalactiae, C. avidum, and others.
Discussion: By culturing along the fistula tract, we isolated bacterial strains from multiple sites along the fistula. This study validates our culture methods using fresh and frozen specimens, which will be useful for batch analysis from stored samples. While perianal fistulas are thought to originate in the rectum, these results show both intestinal and skin-colonizing bacteria isolated from both sides of the fistula from the rectal and skin opening. These strains may be involved in the pathogenesis or maintenance of perianal fistulas. Future work will characterize individual strains and use longitudinal samples to characterize the fistula microbiome.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Felix D. Rozenberg, MD1, Samuel Pan, MD2, Joshua Lacoste, BA2, Elisabeth Giselbrecht, 2, Serre-yu Wong, MD, PhD2. P2678 - Mapping Culturable Microbes of Perianal Fistula in Patients With Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Perianal fistulizing Crohn’s disease (PFCD) is a severe manifestation of Crohn’s disease (CD). The fistula microbiome has been shown to be unique in patients with PFCD. However, the role of individual microbes in fistula pathogenesis remains unexplored. To describe and obtain bacterial species of fistula tracts for mechanistic studies, we aim to establish broad culture of bacteria from perianal fistulas and evaluate changes in the fistula microbiome relative to disease outcomes.
Methods: We conducted a prospective observational study of 80 adult patients with perianal disease undergoing exam under anesthesia (EUA). During EUA, specimens were collected from three sites of the fistula tunnels: (1) swab of perianal skin surrounding the external opening, (2) brushing of fistula tract, and (3) brushing of the inner opening in the rectum. Samples from two patients with both freshly collected and frozen samples were compared. Samples were plated and grown in anaerobic, microaerophilic, and aerobic conditions. Individual colonies were picked for strain identification by MALDI-TOF.
Results: Of the 80 patients, 62 (77.5%) had PFCD, 7 (8.8%) had ileal pouch-anal anastomosis fistulas, and 11 (13.8%) were non-IBD controls. We further collected longitudinal samples from 10 adults with PFCD and one with a non-CD fistula. Table 1 describes the disease progression of these patients between sample collection dates.
Here, we show data from culturing specimens from two patients. The bacterial strains cultured from within the fistula were a mix of intestinal and skin-colonizing bacteria (Figure 1). Similar strains were cultured from both fresh and frozen specimens. Multiple bacterial strains commonly known to colonize skin were cultured from both the internal and external fistula opening brushings, such as S. aureus, S. dysgalactiae, C. avidum, and others.
Discussion: By culturing along the fistula tract, we isolated bacterial strains from multiple sites along the fistula. This study validates our culture methods using fresh and frozen specimens, which will be useful for batch analysis from stored samples. While perianal fistulas are thought to originate in the rectum, these results show both intestinal and skin-colonizing bacteria isolated from both sides of the fistula from the rectal and skin opening. These strains may be involved in the pathogenesis or maintenance of perianal fistulas. Future work will characterize individual strains and use longitudinal samples to characterize the fistula microbiome.
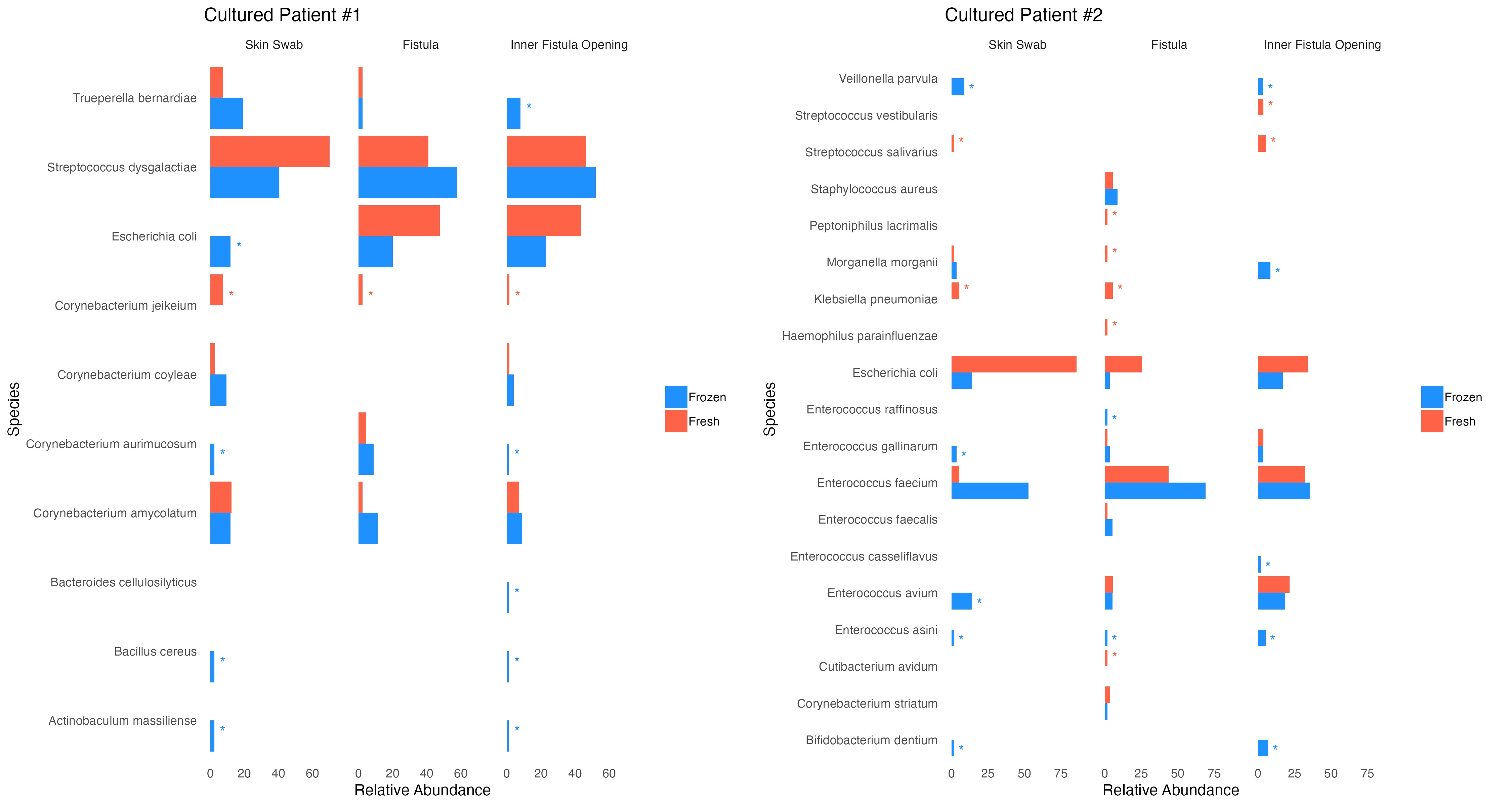
Figure: Bacterial Isolates cultured from three site collection along perianal fistula.
Red * represents strains that were identified in fresh cultures, but not in frozen
Blue * represents strains that were identified in frozen cultures, but not in fresh
Red * represents strains that were identified in fresh cultures, but not in frozen
Blue * represents strains that were identified in frozen cultures, but not in fresh
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Felix Rozenberg indicated no relevant financial relationships.
Samuel Pan indicated no relevant financial relationships.
Joshua Lacoste indicated no relevant financial relationships.
Elisabeth Giselbrecht indicated no relevant financial relationships.
Serre-yu Wong: BMS – Advisory Committee/Board Member. Takeda/Trinetx – Grant/Research Support.
Felix D. Rozenberg, MD1, Samuel Pan, MD2, Joshua Lacoste, BA2, Elisabeth Giselbrecht, 2, Serre-yu Wong, MD, PhD2. P2678 - Mapping Culturable Microbes of Perianal Fistula in Patients With Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
