Monday Poster Session
Category: IBD
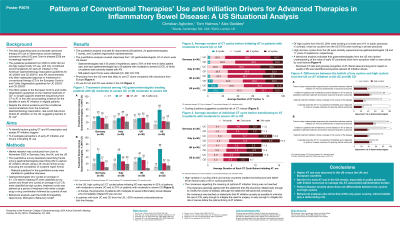
P2679 - Patterns of Conventional Therapies’ Use and Initiation Drivers for Advanced Therapies in Inflammatory Bowel Disease: A US Situational Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Christian Agboton, MD
Takeda
Cambridge, MA
Presenting Author(s)
Christian Agboton, MD1, Tom Halmos, 2, Alex Geddes, PhD2
1Takeda, Cambridge, MA; 2IQVIA, London, England, United Kingdom
Introduction: Despite the clinical evidence for early and broader advanced therapy (AT) use in inflammatory bowel diseases (IBD), actual AT usage remains limited. We evaluated AT use barriers in IBD using multimodal approach to assess if conventional therapy (CT) cycling and AT benefit/risk misperception could explain these barriers.
Methods: Market research was conducted 06/2023–11/2023. Qualitative interviews identified relevant questions for the quantitative survey, which assessed prescribing trends among gastroenterologists (GEs) prescribing ATs to capture AT initiation drivers in Germany, Italy, UK, and US. GEs cycling an average of ≥ 2 CTs before initiating AT were classified as high and 0–1 CTs as low cyclers. Behavioral analysis used the COM-B (Capability, Opportunity, Motivation, Behavior) model.
Results: Qualitative analysis included 62 respondents (28 patients, 24 GEs, 7 nurses, 3 patient organization representatives). Quantitative analysis covered responses from 142 GEs (52 US-based) currently prescribing ATs; 559 patient report forms were collected (ulcerative colitis [UC], 280; Crohn’s disease [CD], 279). US physicians were less likely to use CT alone vs European physicians; AT use for UC and CD was similar in the US (Table). Of US physicians, high cycling was reported by 52%/37% for UC/CD. In both UC and CD, > 50% of patients received corticosteroids as first-line therapy. In all countries including US, the 2 main reasons for early AT initiation were severe individual complications and severe quality of life (QoL) impact, illustrating the prevalence of the “fail first” attitude. Most low cyclers in US (75%), but not European countries, were in private practices. GEs without dedicated staff to handle insurer authorizations were less likely to initiate AT early. Behavioral analysis indicated that GEs who lacked understanding of the value of early AT prioritized short-term symptom relief or were driven by cost factors. Perceived CT risks and growing recognition of AT clinical value and long-term QoL impact were identified as physician-relevant AT initiation drivers. Patient-relevant drivers included improved AT awareness and the patient ability and confidence to self-advocate.
Discussion: A higher AT use was observed in US vs UK and European countries. Barriers for early AT use remain, especially in public practices with limited resources to manage the AT-associated administrative burden. Behavioral analyses also show that within any given country, clinical beliefs play a determining role.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Christian Agboton, MD1, Tom Halmos, 2, Alex Geddes, PhD2. P2679 - Patterns of Conventional Therapies’ Use and Initiation Drivers for Advanced Therapies in Inflammatory Bowel Disease: A US Situational Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Takeda, Cambridge, MA; 2IQVIA, London, England, United Kingdom
Introduction: Despite the clinical evidence for early and broader advanced therapy (AT) use in inflammatory bowel diseases (IBD), actual AT usage remains limited. We evaluated AT use barriers in IBD using multimodal approach to assess if conventional therapy (CT) cycling and AT benefit/risk misperception could explain these barriers.
Methods: Market research was conducted 06/2023–11/2023. Qualitative interviews identified relevant questions for the quantitative survey, which assessed prescribing trends among gastroenterologists (GEs) prescribing ATs to capture AT initiation drivers in Germany, Italy, UK, and US. GEs cycling an average of ≥ 2 CTs before initiating AT were classified as high and 0–1 CTs as low cyclers. Behavioral analysis used the COM-B (Capability, Opportunity, Motivation, Behavior) model.
Results: Qualitative analysis included 62 respondents (28 patients, 24 GEs, 7 nurses, 3 patient organization representatives). Quantitative analysis covered responses from 142 GEs (52 US-based) currently prescribing ATs; 559 patient report forms were collected (ulcerative colitis [UC], 280; Crohn’s disease [CD], 279). US physicians were less likely to use CT alone vs European physicians; AT use for UC and CD was similar in the US (Table). Of US physicians, high cycling was reported by 52%/37% for UC/CD. In both UC and CD, > 50% of patients received corticosteroids as first-line therapy. In all countries including US, the 2 main reasons for early AT initiation were severe individual complications and severe quality of life (QoL) impact, illustrating the prevalence of the “fail first” attitude. Most low cyclers in US (75%), but not European countries, were in private practices. GEs without dedicated staff to handle insurer authorizations were less likely to initiate AT early. Behavioral analysis indicated that GEs who lacked understanding of the value of early AT prioritized short-term symptom relief or were driven by cost factors. Perceived CT risks and growing recognition of AT clinical value and long-term QoL impact were identified as physician-relevant AT initiation drivers. Patient-relevant drivers included improved AT awareness and the patient ability and confidence to self-advocate.
Discussion: A higher AT use was observed in US vs UK and European countries. Barriers for early AT use remain, especially in public practices with limited resources to manage the AT-associated administrative burden. Behavioral analyses also show that within any given country, clinical beliefs play a determining role.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Christian Agboton: Takeda – Employee, Stock Options.
Tom Halmos: IQVIA – Employee.
Alex Geddes: IQVIA – Employee.
Christian Agboton, MD1, Tom Halmos, 2, Alex Geddes, PhD2. P2679 - Patterns of Conventional Therapies’ Use and Initiation Drivers for Advanced Therapies in Inflammatory Bowel Disease: A US Situational Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
