Monday Poster Session
Category: IBD
P2689 - Examining the 1-Year Risk of Cardiovascular Outcomes of TNF-Alpha Inhibitors Among IBD Patients
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SG
Sanya Goswami, MD
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Sanya Goswami, MD1, Rahul Raiker, MD2, Nanda Siva, MBA3, Haig Pakhchanian, MD4, Justin T.. Kupec, MD5
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2George Washington University School of Medicine and Health Sciences, Washington, DC; 3West Virginia University School of Medicine, Morgantown, WV; 4RWJBarnabas Health, Toms River, NJ; 5West Virginia University, Morgantown, WV
Introduction: Inflammatory bowel disease (IBD) a chronic inflammatory disease of the gastrointestinal tract with extraintestinal manifestations, can be managed effectively with tumor necrosis factor inhibitors (TNFi). Incident heart failure has been noted as a rare adverse side effect of TNFi. However, data on assessing HF risk has been mixed with most studies being conducted among rheumatoid arthritis patients. No large studies have assessed this risk among IBD patients on TNFi and therefore the aim was to examine the cardiovascular implications of incident HF and HF exacerbation among IBD patients on TNFi.
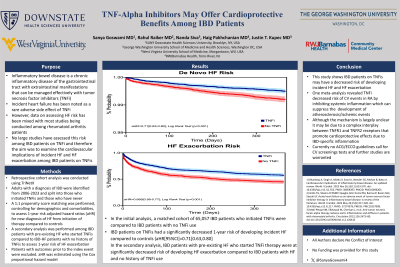
Methods: A retrospective cohort analysis was conducted using TriNetX, a federated database of ~110 million patients across 80 healthcare organizations. Adults with a diagnosis of IBD were identified from 2006-2023 and split into those who initiated TNFi’s and those who have never been on TNFi’s. A 1:1 propensity score matching was performed, controlling for demographics and comorbidities, to assess 1-year risk adjusted hazard ratios (aHR) for new diagnosis of HF from initiation of therapy compared to controls. A secondary analysis was performed among IBD patients with pre-existing HF who started TNFi’s compared to IBD-HF patients with no history of TNFi’s to assess 1-year risk of HF exacerbation. Patients with outcomes prior to the index event were excluded. aHR was estimated using the Cox proportional hazard model.
Results: In the initial analysis, a matched cohort of 65,057 IBD patients who initiated TNFi’s were compared to IBD patients with no TNFi use. IBD patients on TNFi’s had a significantly decreased 1-year risk of developing incident HF compared to controls (aHR[95%CI]=0.71[0.63,0.80]). In the secondary analysis, IBD patients with pre-existing HF who started TNFi therapy were at significantly decreased risk of developing HF exacerbation compared to IBD patients with HF and no history of TNFi use (0.654[0.53,0.81]).
Discussion: This study shows that IBD patients on TNFi’s may have a decreased risk of developing incident HF and exacerbations of HF. Although the mechanism is unclear, it may be due to a complex interplay between TNFR1 and TNFR2 receptors that promote cardioprotective effects due to IBD-specific inflammation. Further studies are warranted to validate these findings for better assessment on recommendations.
Disclosures:
Sanya Goswami, MD1, Rahul Raiker, MD2, Nanda Siva, MBA3, Haig Pakhchanian, MD4, Justin T.. Kupec, MD5. P2689 - Examining the 1-Year Risk of Cardiovascular Outcomes of TNF-Alpha Inhibitors Among IBD Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2George Washington University School of Medicine and Health Sciences, Washington, DC; 3West Virginia University School of Medicine, Morgantown, WV; 4RWJBarnabas Health, Toms River, NJ; 5West Virginia University, Morgantown, WV
Introduction: Inflammatory bowel disease (IBD) a chronic inflammatory disease of the gastrointestinal tract with extraintestinal manifestations, can be managed effectively with tumor necrosis factor inhibitors (TNFi). Incident heart failure has been noted as a rare adverse side effect of TNFi. However, data on assessing HF risk has been mixed with most studies being conducted among rheumatoid arthritis patients. No large studies have assessed this risk among IBD patients on TNFi and therefore the aim was to examine the cardiovascular implications of incident HF and HF exacerbation among IBD patients on TNFi.
Methods: A retrospective cohort analysis was conducted using TriNetX, a federated database of ~110 million patients across 80 healthcare organizations. Adults with a diagnosis of IBD were identified from 2006-2023 and split into those who initiated TNFi’s and those who have never been on TNFi’s. A 1:1 propensity score matching was performed, controlling for demographics and comorbidities, to assess 1-year risk adjusted hazard ratios (aHR) for new diagnosis of HF from initiation of therapy compared to controls. A secondary analysis was performed among IBD patients with pre-existing HF who started TNFi’s compared to IBD-HF patients with no history of TNFi’s to assess 1-year risk of HF exacerbation. Patients with outcomes prior to the index event were excluded. aHR was estimated using the Cox proportional hazard model.
Results: In the initial analysis, a matched cohort of 65,057 IBD patients who initiated TNFi’s were compared to IBD patients with no TNFi use. IBD patients on TNFi’s had a significantly decreased 1-year risk of developing incident HF compared to controls (aHR[95%CI]=0.71[0.63,0.80]). In the secondary analysis, IBD patients with pre-existing HF who started TNFi therapy were at significantly decreased risk of developing HF exacerbation compared to IBD patients with HF and no history of TNFi use (0.654[0.53,0.81]).
Discussion: This study shows that IBD patients on TNFi’s may have a decreased risk of developing incident HF and exacerbations of HF. Although the mechanism is unclear, it may be due to a complex interplay between TNFR1 and TNFR2 receptors that promote cardioprotective effects due to IBD-specific inflammation. Further studies are warranted to validate these findings for better assessment on recommendations.
Disclosures:
Sanya Goswami indicated no relevant financial relationships.
Rahul Raiker indicated no relevant financial relationships.
Nanda Siva indicated no relevant financial relationships.
Haig Pakhchanian indicated no relevant financial relationships.
Justin Kupec indicated no relevant financial relationships.
Sanya Goswami, MD1, Rahul Raiker, MD2, Nanda Siva, MBA3, Haig Pakhchanian, MD4, Justin T.. Kupec, MD5. P2689 - Examining the 1-Year Risk of Cardiovascular Outcomes of TNF-Alpha Inhibitors Among IBD Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
