Monday Poster Session
Category: Interventional Endoscopy
P2743 - Bowel Obstruction due to Enteral and Hepatobiliary Stent Migration: A Systematic Review
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Abdellatif Ismail, MD
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Abdellatif Ismail, MD1, Mohanad Awadalla, MD2, Shaikhoon S. Mohammed, MD3, Khalid Aloum, MD4, Ayman Elawad, MD5, Mohammad Adam, MD, MSc6, Hazem Abosheaishaa, MD7, Monzer Abdalla, MD8, Khalid Ahmed, MD9, Natalie Wilson, MD10, Mohamed Abdallah, MD11, Mohammad Bilal, MD12, Prabhleen Chahal, MD13
1University of Maryland Medical Center, Baltimore, MD; 2Beth Israel Deaconess Medical Center, Boston, MA; 3Emory Clinic/Emory Healthcare, Atlanta, GA; 4St. Barnabas Hospital, Bronx, NY; 5Massachusetts General Hospital, Boston, MA; 6University of Missouri - Kansas City School of Medicine, Kansas City, MO; 7Icahn School of Medicine at Mount Sinai, Queens, NY; 8Ascension Saint Francis Hospital, Evanston, IL; 9University of Pennsylvania, Philadelphia, PA; 10University of Minnesota, Minneapolis, MN; 11Cleveland Clinic, Cleveland, OH; 12University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 13Cleveland Clinic Foundation, Cleveland, OH
Introduction: Enteral and hepatobiliary stents (gastrointestinal (GI) stents) are a useful tool in the armamentarium of endoscopists. Migration of these stents can happen with, most stents passing through the intestine without adverse events (AEs), however, bowel obstruction (BO) has been reported in a few cases. In this comprehensive review of the literature, we aim to explore BO following GI stent migration.
Methods: A comprehensive literature search was conducted in all databases through April 2024 for cases of BO caused by GI stent migration. The outcome of interest was small or large BO resulting from stent migration. We collected data on patient and procedural characteristics, as well as clinical outcomes. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines to identify full-length articles in English language.
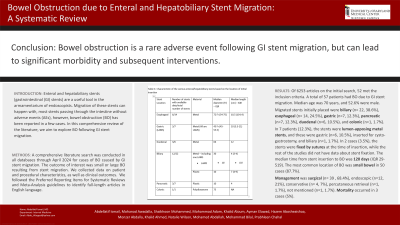
Results: Of 6253 articles on the initial search, 52 met the inclusion criteria. All studies were case reports/series except two prospective and one retrospective cohort studies. A total of 57 patients had BO due to GI stent migration. Median age was 70 years (IQR 58-80), and 52.6% were male. A total of 23 patients (40.3%) had a history of abdominal surgery, and 23 patients (40.3%) had a history of abdominal or pelvic cancer.
Migrated stents initially placed were biliary (n= 22, 38.6%), esophageal (n= 14, 24.5%), gastric (n=7, 12.3%), pancreatic (n=7, 12.3%), duodenal (n=6, 10.5%), and colonic (n=1, 1.7%).
In 7 patients (12.3%), the stents were lumen-apposing metal stents, and these were gastric (n=6, 10.5%), inserted for cysto-gastrostomy, and biliary (n=1, 1.7%). In 2 cases (3.5%), the stents were fixed by sutures at the time of insertion, while the rest of the studies did not have data about stent fixation. Further stent characteristics are summarized in Table 1. The median time from stent insertion to BO was 120 days (IQR 29-519). The most common location of BO was small bowel in 50 cases (87.7%).
Management was as follows: surgical 39 (68.4%), endoscopic 12 (21%), conservative 4 (7%), percutaneous retrieval 1 (1.7%), not mentioned 1 (1.7%).
The median hospital length of stay was 7.5 days (IQR 4-9.5). Mortality occurred in 3 cases (5%).
Discussion: BO is a rare AE following GI stent migration, but can lead to significant morbidity and subsequent interventions.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abdellatif Ismail, MD1, Mohanad Awadalla, MD2, Shaikhoon S. Mohammed, MD3, Khalid Aloum, MD4, Ayman Elawad, MD5, Mohammad Adam, MD, MSc6, Hazem Abosheaishaa, MD7, Monzer Abdalla, MD8, Khalid Ahmed, MD9, Natalie Wilson, MD10, Mohamed Abdallah, MD11, Mohammad Bilal, MD12, Prabhleen Chahal, MD13. P2743 - Bowel Obstruction due to Enteral and Hepatobiliary Stent Migration: A Systematic Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Maryland Medical Center, Baltimore, MD; 2Beth Israel Deaconess Medical Center, Boston, MA; 3Emory Clinic/Emory Healthcare, Atlanta, GA; 4St. Barnabas Hospital, Bronx, NY; 5Massachusetts General Hospital, Boston, MA; 6University of Missouri - Kansas City School of Medicine, Kansas City, MO; 7Icahn School of Medicine at Mount Sinai, Queens, NY; 8Ascension Saint Francis Hospital, Evanston, IL; 9University of Pennsylvania, Philadelphia, PA; 10University of Minnesota, Minneapolis, MN; 11Cleveland Clinic, Cleveland, OH; 12University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 13Cleveland Clinic Foundation, Cleveland, OH
Introduction: Enteral and hepatobiliary stents (gastrointestinal (GI) stents) are a useful tool in the armamentarium of endoscopists. Migration of these stents can happen with, most stents passing through the intestine without adverse events (AEs), however, bowel obstruction (BO) has been reported in a few cases. In this comprehensive review of the literature, we aim to explore BO following GI stent migration.
Methods: A comprehensive literature search was conducted in all databases through April 2024 for cases of BO caused by GI stent migration. The outcome of interest was small or large BO resulting from stent migration. We collected data on patient and procedural characteristics, as well as clinical outcomes. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines to identify full-length articles in English language.
Results: Of 6253 articles on the initial search, 52 met the inclusion criteria. All studies were case reports/series except two prospective and one retrospective cohort studies. A total of 57 patients had BO due to GI stent migration. Median age was 70 years (IQR 58-80), and 52.6% were male. A total of 23 patients (40.3%) had a history of abdominal surgery, and 23 patients (40.3%) had a history of abdominal or pelvic cancer.
Migrated stents initially placed were biliary (n= 22, 38.6%), esophageal (n= 14, 24.5%), gastric (n=7, 12.3%), pancreatic (n=7, 12.3%), duodenal (n=6, 10.5%), and colonic (n=1, 1.7%).
In 7 patients (12.3%), the stents were lumen-apposing metal stents, and these were gastric (n=6, 10.5%), inserted for cysto-gastrostomy, and biliary (n=1, 1.7%). In 2 cases (3.5%), the stents were fixed by sutures at the time of insertion, while the rest of the studies did not have data about stent fixation. Further stent characteristics are summarized in Table 1. The median time from stent insertion to BO was 120 days (IQR 29-519). The most common location of BO was small bowel in 50 cases (87.7%).
Management was as follows: surgical 39 (68.4%), endoscopic 12 (21%), conservative 4 (7%), percutaneous retrieval 1 (1.7%), not mentioned 1 (1.7%).
The median hospital length of stay was 7.5 days (IQR 4-9.5). Mortality occurred in 3 cases (5%).
Discussion: BO is a rare AE following GI stent migration, but can lead to significant morbidity and subsequent interventions.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abdellatif Ismail indicated no relevant financial relationships.
Mohanad Awadalla indicated no relevant financial relationships.
Shaikhoon Mohammed indicated no relevant financial relationships.
Khalid Aloum indicated no relevant financial relationships.
Ayman Elawad indicated no relevant financial relationships.
Mohammad Adam indicated no relevant financial relationships.
Hazem Abosheaishaa indicated no relevant financial relationships.
Monzer Abdalla indicated no relevant financial relationships.
Khalid Ahmed indicated no relevant financial relationships.
Natalie Wilson indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Prabhleen Chahal: Boston Scientific – Advisor or Review Panel Member.
Abdellatif Ismail, MD1, Mohanad Awadalla, MD2, Shaikhoon S. Mohammed, MD3, Khalid Aloum, MD4, Ayman Elawad, MD5, Mohammad Adam, MD, MSc6, Hazem Abosheaishaa, MD7, Monzer Abdalla, MD8, Khalid Ahmed, MD9, Natalie Wilson, MD10, Mohamed Abdallah, MD11, Mohammad Bilal, MD12, Prabhleen Chahal, MD13. P2743 - Bowel Obstruction due to Enteral and Hepatobiliary Stent Migration: A Systematic Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
