Monday Poster Session
Category: Interventional Endoscopy
P2750 - Comparative Efficacy and Safety of Endoscopic Submucosal Dissection versus Endoscopic Mucosal Resection for Gastrointestinal Lesions: A Meta-Analysis and Systematic Review
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nouman Shafique, MD
AdventHealth Medical Group, AdventHealth
Orlando, FL
Presenting Author(s)
Nouman Shafique, MD1, Ali Raza Khan, MBBS2, Fnu Muhibullah, MD, MBBS3, Shahzad Zafar, MBBS2, Abdul Qadeer, 2, Adeena Shafique, 4, Iqra Shafiq, MBBS5, Babu Mohan, MD6
1AdventHealth Medical Group, AdventHealth, Orlando, FL; 2Nishtar Medical University, Multan, Punjab, Pakistan; 3West Virginia University Camden Clark Medical Center, Parkersburg, WV; 4Aga Khan University, Karachi, Sindh, Pakistan; 5Combined Military Hospital, Bahawalpur, Punjab, Pakistan; 6Orlando Gastroenterology PA, Orlando, FL
Introduction: Endoscopic submucosal dissection (ESD) and endoscopic mucosal resection (EMR) are widely used techniques in the endoscopic treatment of gastrointestinal lesions. The high risk of complications associated with these procedures remains a concern. The aim of our study was to evaluate and compare the efficacy and safety of ESD and EMR for treating gastrointestinal lesions and across multiple clinical outcomes.
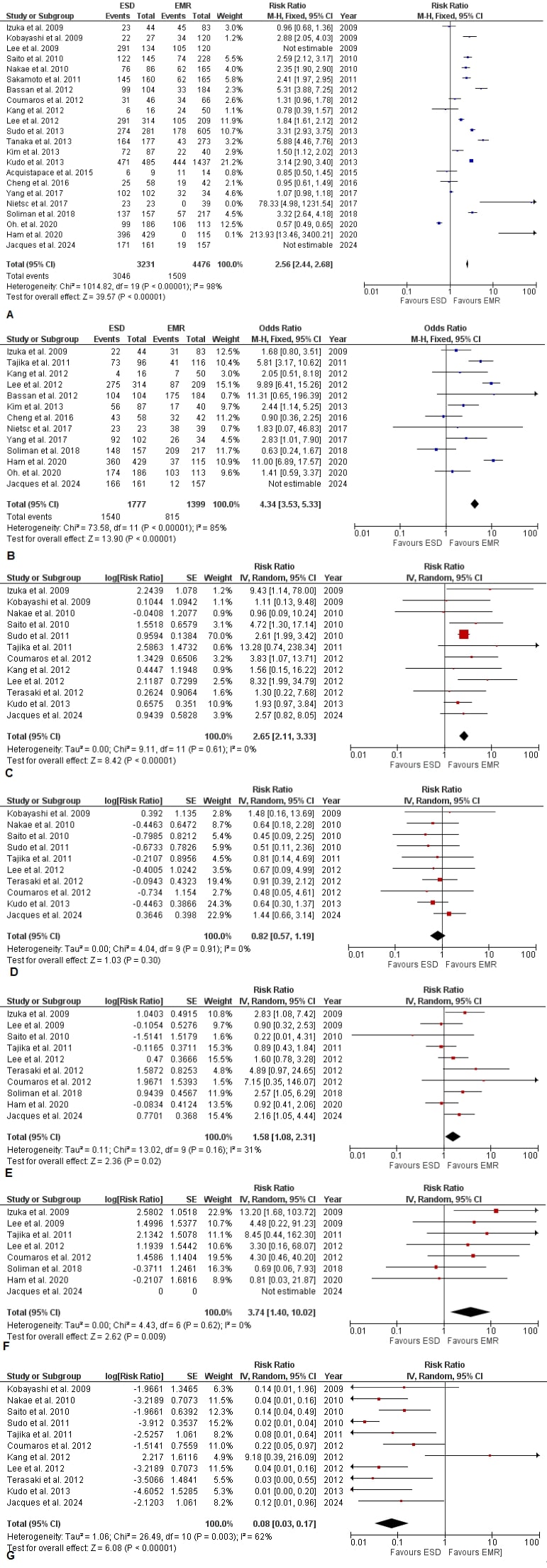
Methods: A comprehensive literature search was conducted using PubMed, EMBASE, and Cochrane Library to identify studies comparing ESD and EMR. Relevant studies were included, and data were extracted and analyzed using a random-effects model. The primary endpoints were post-procedural bleeding, perforation rates, rates of surgery for oncologic adequacy, recurrence rates, R0 resection rates, surgery for complications, and en-bloc resection rates. Forest plots were generated to visualize the risk ratios (RR) and confidence intervals (CI) for each outcome.
Results: We included 22 studies including 7,707 patients. There were 3,231 patients in ESD group and 4, 476 patients in the EMR group. There was a statistically significant higher en-bloc resection rate in patients undergoing ESD compared to EMR (RR: 2.56 [2.44; 2.68]; I²=98%; p < 0.001). The R0 resection rate was also significantly higher for ESD (RR: 4.34 [3.53; 5.33]; I²=85%; p < 0.001). The rate of perforation was significantly higher in the ESD group (RR: 2.65 [2.11; 3.33]; I²=0%; p < 0.001), while the rate of post-procedural bleeding showed no significant difference between ESD and EMR (RR: 0.82 [0.57; 1.19]; I²=0%; p = 0.30). The overall need for further surgery, including surgery for oncologic reasons and complications, was higher in the ESD group (RR: 1.58 [1.08; 2.31]; I²=31%; p = 0.02). Recurrence rates were significantly lower in the ESD group (RR: 0.08 [0.03; 0.17]; I²=62%; p < 0.001).
Discussion: Our meta-analysis underscores the superiority of ESD over EMR in terms of oncologic outcomes, particularly in achieving significantly higher en-bloc and R0 resection rates and lower recurrence rates. However, the higher risk of perforation and the increased need for further surgery due to complications associated with ESD cannot be ignored. These results emphasize the necessity for careful patient selection and the development of risk management strategies when considering ESD as a treatment option. Further research is warranted to enhance the safety and efficacy of ESD in clinical practice
Disclosures:
Nouman Shafique, MD1, Ali Raza Khan, MBBS2, Fnu Muhibullah, MD, MBBS3, Shahzad Zafar, MBBS2, Abdul Qadeer, 2, Adeena Shafique, 4, Iqra Shafiq, MBBS5, Babu Mohan, MD6. P2750 - Comparative Efficacy and Safety of Endoscopic Submucosal Dissection versus Endoscopic Mucosal Resection for Gastrointestinal Lesions: A Meta-Analysis and Systematic Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1AdventHealth Medical Group, AdventHealth, Orlando, FL; 2Nishtar Medical University, Multan, Punjab, Pakistan; 3West Virginia University Camden Clark Medical Center, Parkersburg, WV; 4Aga Khan University, Karachi, Sindh, Pakistan; 5Combined Military Hospital, Bahawalpur, Punjab, Pakistan; 6Orlando Gastroenterology PA, Orlando, FL
Introduction: Endoscopic submucosal dissection (ESD) and endoscopic mucosal resection (EMR) are widely used techniques in the endoscopic treatment of gastrointestinal lesions. The high risk of complications associated with these procedures remains a concern. The aim of our study was to evaluate and compare the efficacy and safety of ESD and EMR for treating gastrointestinal lesions and across multiple clinical outcomes.
Methods: A comprehensive literature search was conducted using PubMed, EMBASE, and Cochrane Library to identify studies comparing ESD and EMR. Relevant studies were included, and data were extracted and analyzed using a random-effects model. The primary endpoints were post-procedural bleeding, perforation rates, rates of surgery for oncologic adequacy, recurrence rates, R0 resection rates, surgery for complications, and en-bloc resection rates. Forest plots were generated to visualize the risk ratios (RR) and confidence intervals (CI) for each outcome.
Results: We included 22 studies including 7,707 patients. There were 3,231 patients in ESD group and 4, 476 patients in the EMR group. There was a statistically significant higher en-bloc resection rate in patients undergoing ESD compared to EMR (RR: 2.56 [2.44; 2.68]; I²=98%; p < 0.001). The R0 resection rate was also significantly higher for ESD (RR: 4.34 [3.53; 5.33]; I²=85%; p < 0.001). The rate of perforation was significantly higher in the ESD group (RR: 2.65 [2.11; 3.33]; I²=0%; p < 0.001), while the rate of post-procedural bleeding showed no significant difference between ESD and EMR (RR: 0.82 [0.57; 1.19]; I²=0%; p = 0.30). The overall need for further surgery, including surgery for oncologic reasons and complications, was higher in the ESD group (RR: 1.58 [1.08; 2.31]; I²=31%; p = 0.02). Recurrence rates were significantly lower in the ESD group (RR: 0.08 [0.03; 0.17]; I²=62%; p < 0.001).
Discussion: Our meta-analysis underscores the superiority of ESD over EMR in terms of oncologic outcomes, particularly in achieving significantly higher en-bloc and R0 resection rates and lower recurrence rates. However, the higher risk of perforation and the increased need for further surgery due to complications associated with ESD cannot be ignored. These results emphasize the necessity for careful patient selection and the development of risk management strategies when considering ESD as a treatment option. Further research is warranted to enhance the safety and efficacy of ESD in clinical practice
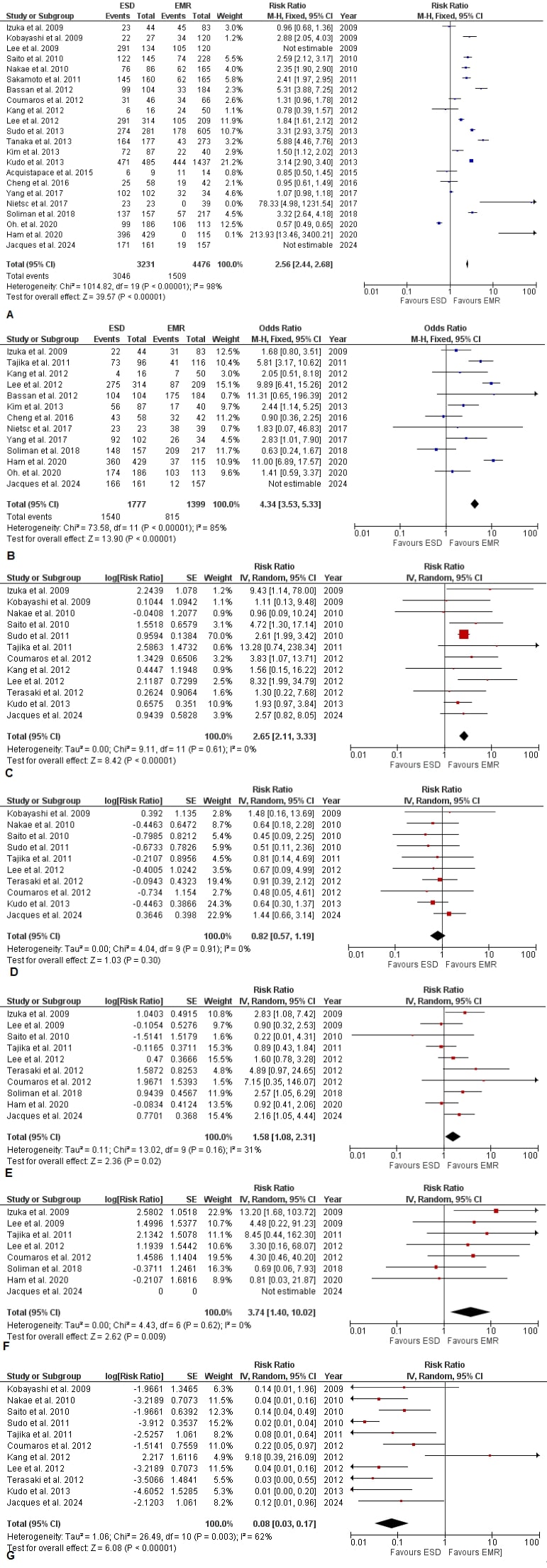
Figure: Figure 1. Forest plot for A) En-bloc Resection Rate B) Ro Resection rate C) Post Procedural Perforation D) Post Procedural Bleeding E) Surgery For Oncologic Reasons F) Surgery For Complications G) Recurrence rate
Disclosures:
Nouman Shafique indicated no relevant financial relationships.
Ali Raza Khan indicated no relevant financial relationships.
Fnu Muhibullah indicated no relevant financial relationships.
Shahzad Zafar indicated no relevant financial relationships.
Abdul Qadeer indicated no relevant financial relationships.
Adeena Shafique indicated no relevant financial relationships.
Iqra Shafiq indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Nouman Shafique, MD1, Ali Raza Khan, MBBS2, Fnu Muhibullah, MD, MBBS3, Shahzad Zafar, MBBS2, Abdul Qadeer, 2, Adeena Shafique, 4, Iqra Shafiq, MBBS5, Babu Mohan, MD6. P2750 - Comparative Efficacy and Safety of Endoscopic Submucosal Dissection versus Endoscopic Mucosal Resection for Gastrointestinal Lesions: A Meta-Analysis and Systematic Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
