Monday Poster Session
Category: Interventional Endoscopy
P2821 - Successful Management of Refractory Esophagojejunal Anastomotic Leak Following Total Gastrectomy Using Endoluminal Vacuum Therapy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Wendy T. Garzon-Siatoya, MD
St. Barnabas Hospital
Bronx, NY
Presenting Author(s)
Wendy T. Garzon-Siatoya, MD1, Kavel H. Visrodia, MD2, Amrita Sethi, MD2
1St. Barnabas Hospital, Bronx, NY; 2New York-Presbyterian/Columbia University Irving Medical Center, New York, NY
Introduction: Complications after total gastrectomy like esophagojejunal (EJ) anastomotic dehiscence historically required surgical revision. However, minimally invasive methods like esophageal clipping, stenting, endoscopic suturing, and endoluminal vacuum therapy (EndoVAC) have been reported. We demonstrate the success of endoscopic suturing, stenting and ultimately EndoVAC in treating a refractory EJ leak.
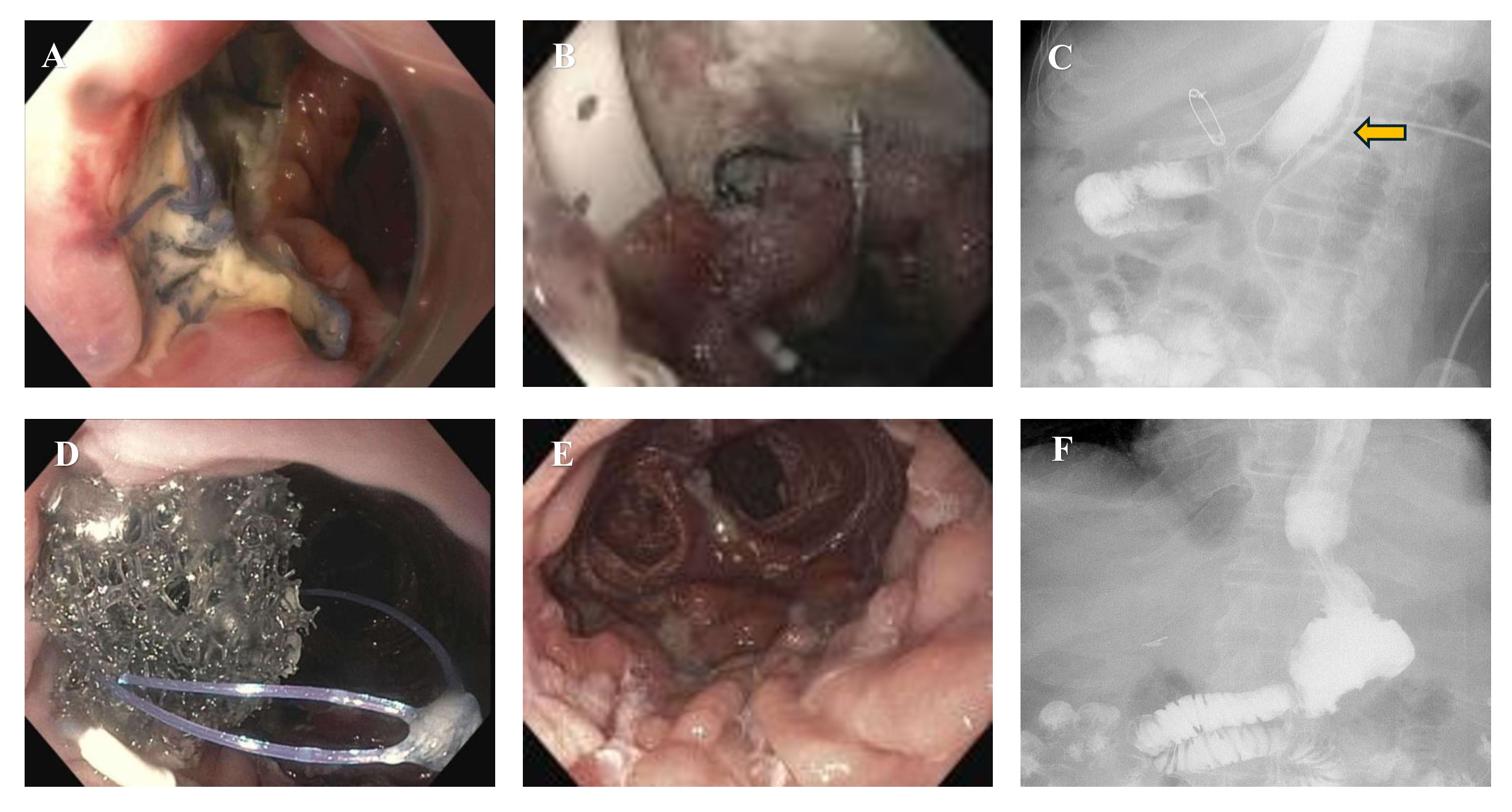
Case Description/Methods: A 79-year-old male with gastric fundal adenocarcinoma underwent open total gastrectomy and omentectomy. On postoperative day (POD) 3 the course was complicated by EJ anastomotic dehiscence, requiring surgical revision with placement of a surgical drain and initiation of parenteral nutrition. However, a persistent leak with dehiscence was suspected and confirmed on POD 15 esophagogastroduodenoscopy (EGD) (Fig.1A) and managed with endoscopic suturing. On POD 22, repeat EGD showed a persistent defect around the intraluminal drain protruding through the EJ, and managed with additional suturing and an esophageal stent (Fig.1B). Subsequent esophagrams showed reduced leak, allowing patient discharge. However, he returned at 2 months with esophagram showing persistent leak (Fig.1C). On repeat EGD, the esophageal stent was removed, revealing the intraluminal drain with decreased but persistent defect. Endoscopic and surgical sutures were removed, and the drain was replaced with an alternate percutaneous drain with limited sideholes (ie, nasogastric tube), covered by a tailored piece of wound vacuum sponge foam. With external traction, the EndoVAC was retracted into the EJ defect and placed on low-intermittent wall suction (80 mmHg) (Fig.1D), with stent replacement. After 1 week, repeat EGD showed budding granulation tissue at the defect, and the EndoVAC was converted from the external drain to an internal nasocystic drain allowing external drain removal, and the esophageal stent was replaced. On final EGD 1 week later, the defect was completely healed (Fig.1E) and esophagram showed a patent EJ without leak or obstruction (Fig.1F) allowing reinitiation of oral intake.
Discussion: EndoVAC can be used to treat challenging refractory gastrointestinal leaks. This case highlights that EndoVAC therapy, although resource intensive, can be a safe and effective tool in managing postoperative anastomotic leaks. Future studies are needed to understand an algorithm to optimize EndoVAC use with respect to other treatment modalities.
Disclosures:
Wendy T. Garzon-Siatoya, MD1, Kavel H. Visrodia, MD2, Amrita Sethi, MD2. P2821 - Successful Management of Refractory Esophagojejunal Anastomotic Leak Following Total Gastrectomy Using Endoluminal Vacuum Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Barnabas Hospital, Bronx, NY; 2New York-Presbyterian/Columbia University Irving Medical Center, New York, NY
Introduction: Complications after total gastrectomy like esophagojejunal (EJ) anastomotic dehiscence historically required surgical revision. However, minimally invasive methods like esophageal clipping, stenting, endoscopic suturing, and endoluminal vacuum therapy (EndoVAC) have been reported. We demonstrate the success of endoscopic suturing, stenting and ultimately EndoVAC in treating a refractory EJ leak.
Case Description/Methods: A 79-year-old male with gastric fundal adenocarcinoma underwent open total gastrectomy and omentectomy. On postoperative day (POD) 3 the course was complicated by EJ anastomotic dehiscence, requiring surgical revision with placement of a surgical drain and initiation of parenteral nutrition. However, a persistent leak with dehiscence was suspected and confirmed on POD 15 esophagogastroduodenoscopy (EGD) (Fig.1A) and managed with endoscopic suturing. On POD 22, repeat EGD showed a persistent defect around the intraluminal drain protruding through the EJ, and managed with additional suturing and an esophageal stent (Fig.1B). Subsequent esophagrams showed reduced leak, allowing patient discharge. However, he returned at 2 months with esophagram showing persistent leak (Fig.1C). On repeat EGD, the esophageal stent was removed, revealing the intraluminal drain with decreased but persistent defect. Endoscopic and surgical sutures were removed, and the drain was replaced with an alternate percutaneous drain with limited sideholes (ie, nasogastric tube), covered by a tailored piece of wound vacuum sponge foam. With external traction, the EndoVAC was retracted into the EJ defect and placed on low-intermittent wall suction (80 mmHg) (Fig.1D), with stent replacement. After 1 week, repeat EGD showed budding granulation tissue at the defect, and the EndoVAC was converted from the external drain to an internal nasocystic drain allowing external drain removal, and the esophageal stent was replaced. On final EGD 1 week later, the defect was completely healed (Fig.1E) and esophagram showed a patent EJ without leak or obstruction (Fig.1F) allowing reinitiation of oral intake.
Discussion: EndoVAC can be used to treat challenging refractory gastrointestinal leaks. This case highlights that EndoVAC therapy, although resource intensive, can be a safe and effective tool in managing postoperative anastomotic leaks. Future studies are needed to understand an algorithm to optimize EndoVAC use with respect to other treatment modalities.
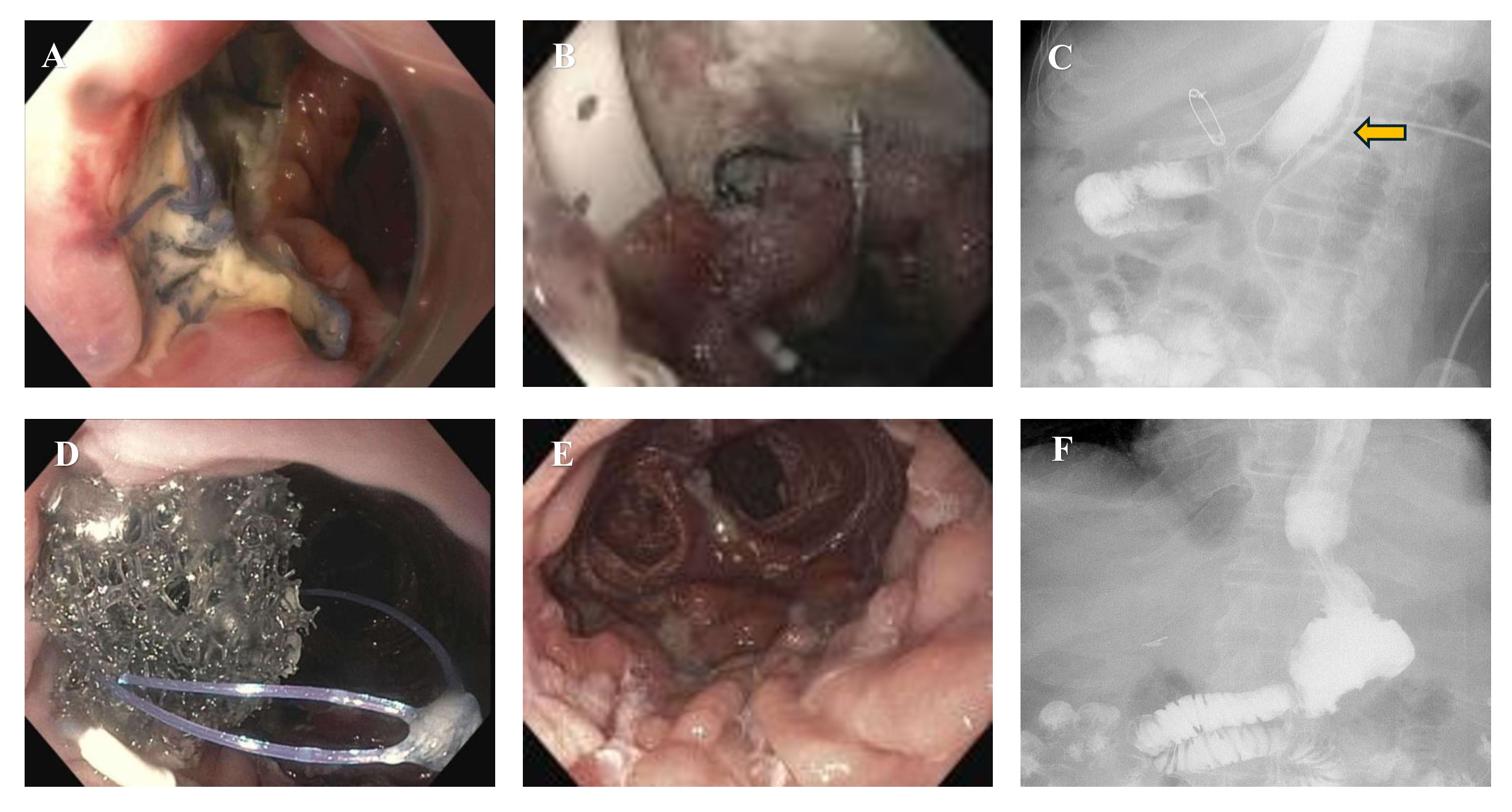
Figure: Figure 1 - A. Esophagogastroduodenoscopy (EGD) showing the esophagojejunal (EJ) anastomotic dehiscence before suturing/stenting. B. EGD post suturing and stenting. C. Esophagram showing persistent leak with contrast through external drain (yellow arrow). D. Endoscopic view of the EndoVAC in place. E. EGD showing final appearance of the EJ defect F. Final esophagram showing absence of leak.
Disclosures:
Wendy Garzon-Siatoya indicated no relevant financial relationships.
Kavel Visrodia indicated no relevant financial relationships.
Amrita Sethi: Boston Scientific – Consultant, Grant/Research Support. Cook Medical – Consultant. Endosound – Advisor or Review Panel Member. ERBE – Grant/Research Support. Fujifilm – Grant/Research Support. Medtronic – Consultant. Olympus – Consultant. Pentax – Consultant.
Wendy T. Garzon-Siatoya, MD1, Kavel H. Visrodia, MD2, Amrita Sethi, MD2. P2821 - Successful Management of Refractory Esophagojejunal Anastomotic Leak Following Total Gastrectomy Using Endoluminal Vacuum Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
