Monday Poster Session
Category: Interventional Endoscopy
P2822 - Endoscopic Papillectomy as a Safe and Effective Treatment for Ampullary Neuroendocrine Tumors: A Case Report
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Wendy T. Garzon-Siatoya, MD
St. Barnabas Hospital
Bronx, NY
Presenting Author(s)
Wendy T. Garzon-Siatoya, MD1, Jason T. Lewis, MD2, Victoria Gómez, MD2
1St. Barnabas Hospital, Bronx, NY; 2Mayo Clinic, Jacksonville, FL
Introduction: Ampullary neuroendocrine tumors (NETs) are rare, comprising less than 1% of all gastrointestinal NETs, and often exhibit high rates of transmural invasion and lymph node metastasis. Although Whipple operation has been the preferred definitive treatment, it carries significant morbidity. Endoscopic papillectomy (EP) has seldom been reported as an alternative treatment option for ampullary NETs. However, the use of EP in this context remains controversial, with no established consensus.
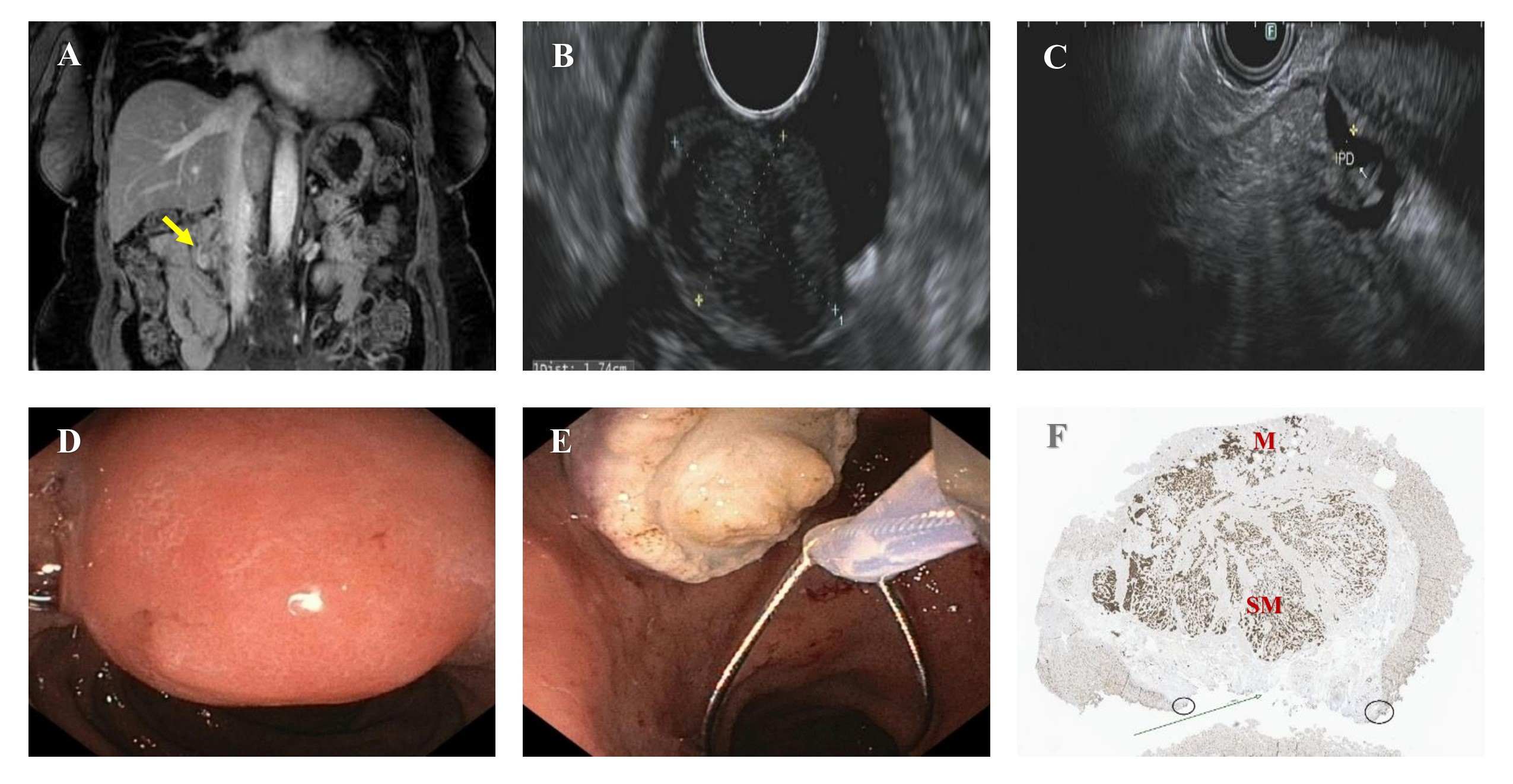
Case Description/Methods: A 58-year-old African American woman with a medical history of hypertension, neurofibromatosis type 1, and a family history of a sister with metastatic NET of the pancreatic head, presented for further evaluation after a screening MRI of the abdomen demonstrated a dilated, tortuous main pancreatic duct measuring up to 7 mm and an enhancing nodular focus at the ampulla protruding into the duodenum (Fig.1A), with no evidence of metastasis. A diagnostic endoscopic ultrasound (EUS) (Fig.1B,1C) identified an oval, hypoechoic subepithelial lesion in the ampulla involving the mucosa and submucosa, measuring 12 mm x 17 mm, and a few lymph nodes at the gastrohepatic ligament were noted. EUS-guided fine needle biopsies of both the ampullary lesion and one lymph node were performed. Pathology showed a well-differentiated NET with a Ki-67 proliferation index of 1%, and the sampled lymph node was negative for malignancy. Given these findings and the absence of invasion or metastasis, the decision was made to proceed with EP instead of surgical intervention. EP was performed, with an en-bloc resection of the lesion using a hot snare through the duodenoscope (Fig.1D,1E). Pathology confirmed a well-differentiated NET (Grade 1), with a Ki-67 proliferation index of 1.2%, measuring 1.2 cm in greatest dimension and invading through the sphincter into the duodenal submucosa. Lymphatic and vascular invasion were not identified. The deep and lateral margins were negative for tumor (Fig.1F). The patient tolerated the procedure well and will return for follow-up in six months for surveillance endoscopy and imaging, given the invasion into the submucosa.
Discussion: EP can potentially serve as an alternative definitive treatment option for localized, well-differentiated ampullary NETs. Furthermore, this case highlights the value of EUS as a complimentary diagnostic study to cross-sectional imaging to evaluate for locoregional metastasis and subepithelial involvement to help guide clinical decision-making.
Disclosures:
Wendy T. Garzon-Siatoya, MD1, Jason T. Lewis, MD2, Victoria Gómez, MD2. P2822 - Endoscopic Papillectomy as a Safe and Effective Treatment for Ampullary Neuroendocrine Tumors: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Barnabas Hospital, Bronx, NY; 2Mayo Clinic, Jacksonville, FL
Introduction: Ampullary neuroendocrine tumors (NETs) are rare, comprising less than 1% of all gastrointestinal NETs, and often exhibit high rates of transmural invasion and lymph node metastasis. Although Whipple operation has been the preferred definitive treatment, it carries significant morbidity. Endoscopic papillectomy (EP) has seldom been reported as an alternative treatment option for ampullary NETs. However, the use of EP in this context remains controversial, with no established consensus.
Case Description/Methods: A 58-year-old African American woman with a medical history of hypertension, neurofibromatosis type 1, and a family history of a sister with metastatic NET of the pancreatic head, presented for further evaluation after a screening MRI of the abdomen demonstrated a dilated, tortuous main pancreatic duct measuring up to 7 mm and an enhancing nodular focus at the ampulla protruding into the duodenum (Fig.1A), with no evidence of metastasis. A diagnostic endoscopic ultrasound (EUS) (Fig.1B,1C) identified an oval, hypoechoic subepithelial lesion in the ampulla involving the mucosa and submucosa, measuring 12 mm x 17 mm, and a few lymph nodes at the gastrohepatic ligament were noted. EUS-guided fine needle biopsies of both the ampullary lesion and one lymph node were performed. Pathology showed a well-differentiated NET with a Ki-67 proliferation index of 1%, and the sampled lymph node was negative for malignancy. Given these findings and the absence of invasion or metastasis, the decision was made to proceed with EP instead of surgical intervention. EP was performed, with an en-bloc resection of the lesion using a hot snare through the duodenoscope (Fig.1D,1E). Pathology confirmed a well-differentiated NET (Grade 1), with a Ki-67 proliferation index of 1.2%, measuring 1.2 cm in greatest dimension and invading through the sphincter into the duodenal submucosa. Lymphatic and vascular invasion were not identified. The deep and lateral margins were negative for tumor (Fig.1F). The patient tolerated the procedure well and will return for follow-up in six months for surveillance endoscopy and imaging, given the invasion into the submucosa.
Discussion: EP can potentially serve as an alternative definitive treatment option for localized, well-differentiated ampullary NETs. Furthermore, this case highlights the value of EUS as a complimentary diagnostic study to cross-sectional imaging to evaluate for locoregional metastasis and subepithelial involvement to help guide clinical decision-making.
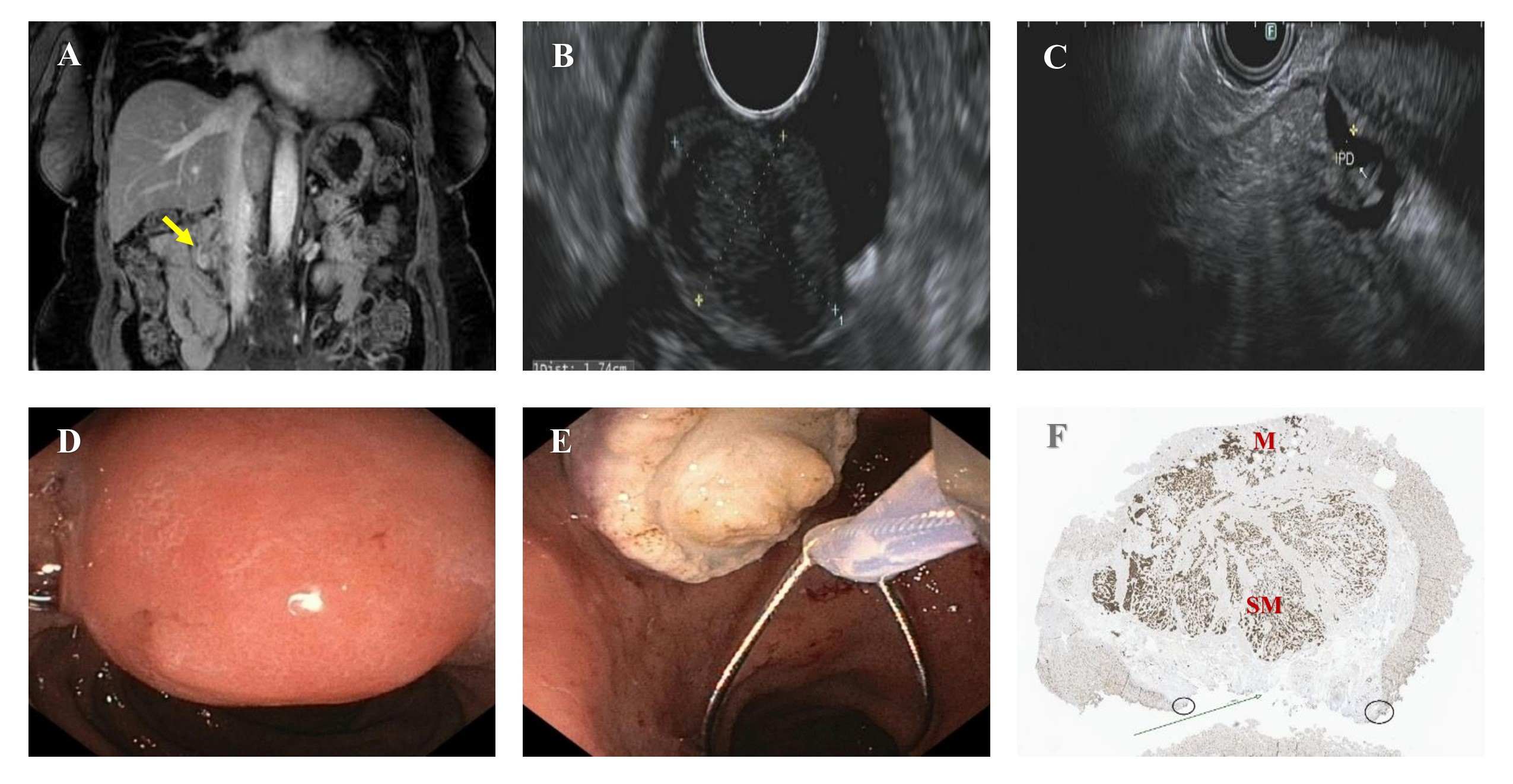
Figure: Figure 1 - A. MRI abdomen showing an enhancing nodular focus at the ampulla protruding into the duodenum (yellow arrow). B. EUS showing an oval, hypoechoic subepithelial lesion in the ampulla, measuring 12 mm x 17 mm, involving the mucosa and submucosa layers. C. EUS showing a dilated pancreatic duct (PD) at the level of the head of pancreas. D. Endoscopic view of the ampullary lesion prior to endoscopic resection. E. Resected ampullary lesion removed with a hot snare. F. En-bloc pathology specimen showing the tumor involving the mucosa (M) and submucosa (SM). The deep (arrow) and lateral margins (circles) are negative for tumor.
Disclosures:
Wendy Garzon-Siatoya indicated no relevant financial relationships.
Jason Lewis indicated no relevant financial relationships.
Victoria Gómez: COOKMedical – Education and Lectures. Olympus – Consultant.
Wendy T. Garzon-Siatoya, MD1, Jason T. Lewis, MD2, Victoria Gómez, MD2. P2822 - Endoscopic Papillectomy as a Safe and Effective Treatment for Ampullary Neuroendocrine Tumors: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
