Monday Poster Session
Category: Interventional Endoscopy
P2840 - Endoscopic Drainage of Intramural Duodenal Hematoma Secondary to Acute Pancreatitis Using Lumen-Apposing Metal Stent (LAMS)
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mohammed Martini, MD
Southern Illinois University
Springfield, IL
Presenting Author(s)
Mohammed Martini, MD1, Medha Rajamanuri, MBBS1, Muaataz Azzawi, MD1, Abdul Swied, MD2
1Southern Illinois University, Springfield, IL; 2Southern Illinois University School of Medicine, Springfield, IL
Introduction: Spontaneous intramural duodenal hematoma (IDH) is an uncommon but significant complication that can arise secondary to acute pancreatitis. While IDH is typically associated with traumatic or iatrogenic injuries, coagulopathies, or bleeding disorders, its occurrence in the context of acute pancreatitis is rare and not well understood. IDH can lead to serious complications, including gastrointestinal obstruction, perforation, and intussusception. Management of IDH varies and can range from conservative treatment to surgical intervention. Here, we present a case of IDH secondary to acute on chronic pancreatitis, managed successfully with endoscopic ultrasound (EUS)-guided drainage.
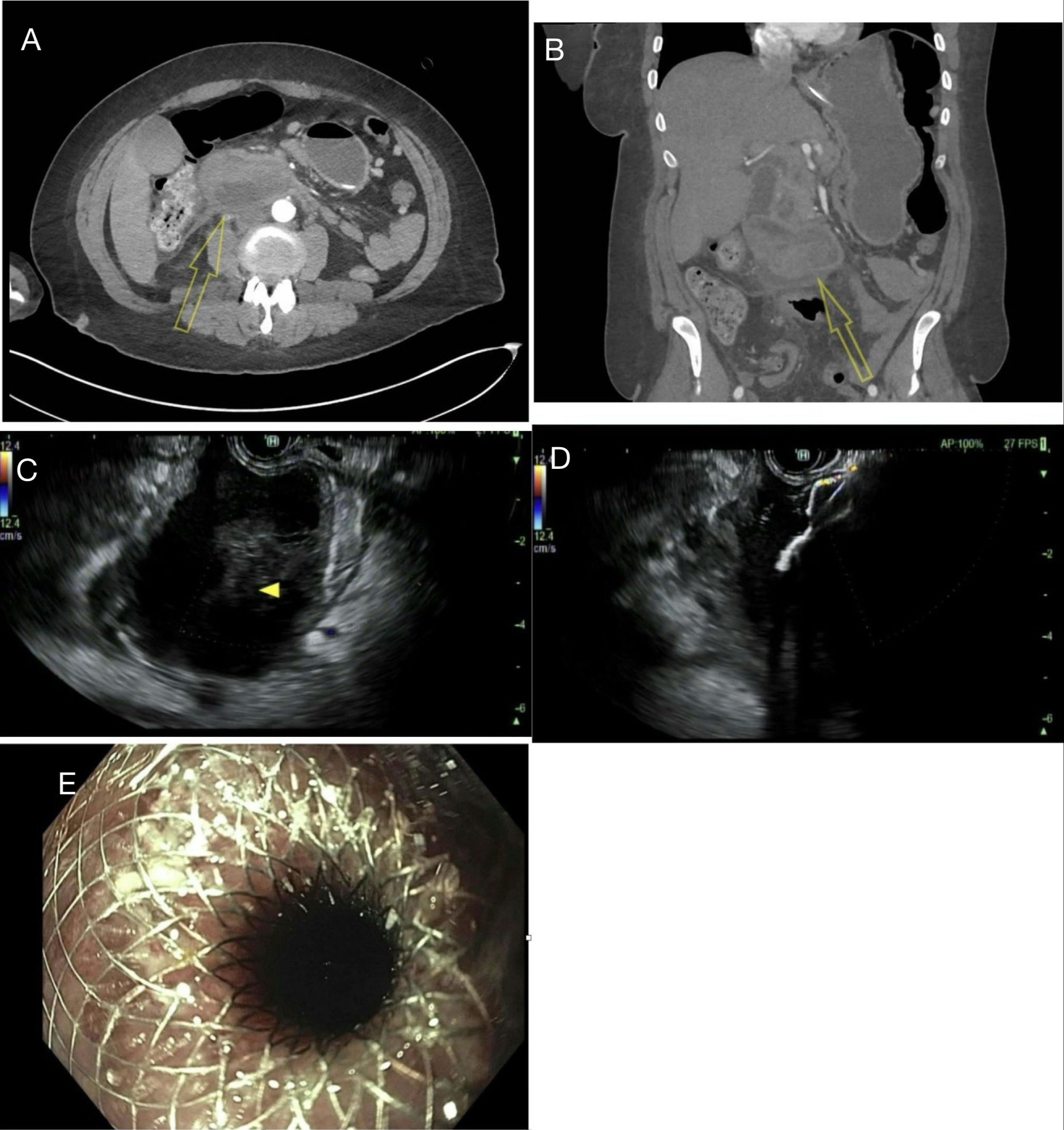
Case Description/Methods: A 41-year-old female with a history of alcohol-associated chronic pancreatitis presented with acute abdominal pain, nausea and vomiting. On examination, she was afebrile and hypertensive with abdominal tenderness. Blood tests showed mild anemia and mild thrombocytopenia. Computed tomography (CT) of the abdomen and pelvis with contrast revealed acute pancreatitis and a large duodenal hematoma of 7 x 5.2 x4.5 cm. Initially, the patient was treated conservatively, but later developed duodenal obstruction. To drain the hematoma internally, we created a cystoduodenostomy using lumen-apposing metal stent (LAMS) guided by the EUS. Subsequently, her symptoms resolved, and she was discharged home. Two weeks later, the stent was removed, and the patient continued to do well on a clinic follow-up.
Discussion: The Relationship between non-traumatic IDH and pancreatitis is not fully understood, proposed mechanisms and leakage of pancreatic enzymes can cause inflammation and local necrosis of the duodenal wall, leading to hematoma formation. Pressure necrosis can cause auto digest and increase vessel permeability which leads to hematoma formation. The patient's history and clinical progression suggested that the duodenal hematoma was a complication of alcohol induced acute pancreatitis. Conservative management is the standard in mildly symptomatic patients, and more invasive interventions may be necessary including percutaneous drainage or surgical treatment in more high-risk cases. However, in some instances, endoscopic decompression such as mucosal resection with fistula construction to facilitate hematoma drainage has been reported as a successful alternative treatment modality. Here we report successful drainage of the IDH with the use of LAMS alone obviating the need for surgical intervention.
Disclosures:
Mohammed Martini, MD1, Medha Rajamanuri, MBBS1, Muaataz Azzawi, MD1, Abdul Swied, MD2. P2840 - Endoscopic Drainage of Intramural Duodenal Hematoma Secondary to Acute Pancreatitis Using Lumen-Apposing Metal Stent (LAMS), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Southern Illinois University, Springfield, IL; 2Southern Illinois University School of Medicine, Springfield, IL
Introduction: Spontaneous intramural duodenal hematoma (IDH) is an uncommon but significant complication that can arise secondary to acute pancreatitis. While IDH is typically associated with traumatic or iatrogenic injuries, coagulopathies, or bleeding disorders, its occurrence in the context of acute pancreatitis is rare and not well understood. IDH can lead to serious complications, including gastrointestinal obstruction, perforation, and intussusception. Management of IDH varies and can range from conservative treatment to surgical intervention. Here, we present a case of IDH secondary to acute on chronic pancreatitis, managed successfully with endoscopic ultrasound (EUS)-guided drainage.
Case Description/Methods: A 41-year-old female with a history of alcohol-associated chronic pancreatitis presented with acute abdominal pain, nausea and vomiting. On examination, she was afebrile and hypertensive with abdominal tenderness. Blood tests showed mild anemia and mild thrombocytopenia. Computed tomography (CT) of the abdomen and pelvis with contrast revealed acute pancreatitis and a large duodenal hematoma of 7 x 5.2 x4.5 cm. Initially, the patient was treated conservatively, but later developed duodenal obstruction. To drain the hematoma internally, we created a cystoduodenostomy using lumen-apposing metal stent (LAMS) guided by the EUS. Subsequently, her symptoms resolved, and she was discharged home. Two weeks later, the stent was removed, and the patient continued to do well on a clinic follow-up.
Discussion: The Relationship between non-traumatic IDH and pancreatitis is not fully understood, proposed mechanisms and leakage of pancreatic enzymes can cause inflammation and local necrosis of the duodenal wall, leading to hematoma formation. Pressure necrosis can cause auto digest and increase vessel permeability which leads to hematoma formation. The patient's history and clinical progression suggested that the duodenal hematoma was a complication of alcohol induced acute pancreatitis. Conservative management is the standard in mildly symptomatic patients, and more invasive interventions may be necessary including percutaneous drainage or surgical treatment in more high-risk cases. However, in some instances, endoscopic decompression such as mucosal resection with fistula construction to facilitate hematoma drainage has been reported as a successful alternative treatment modality. Here we report successful drainage of the IDH with the use of LAMS alone obviating the need for surgical intervention.
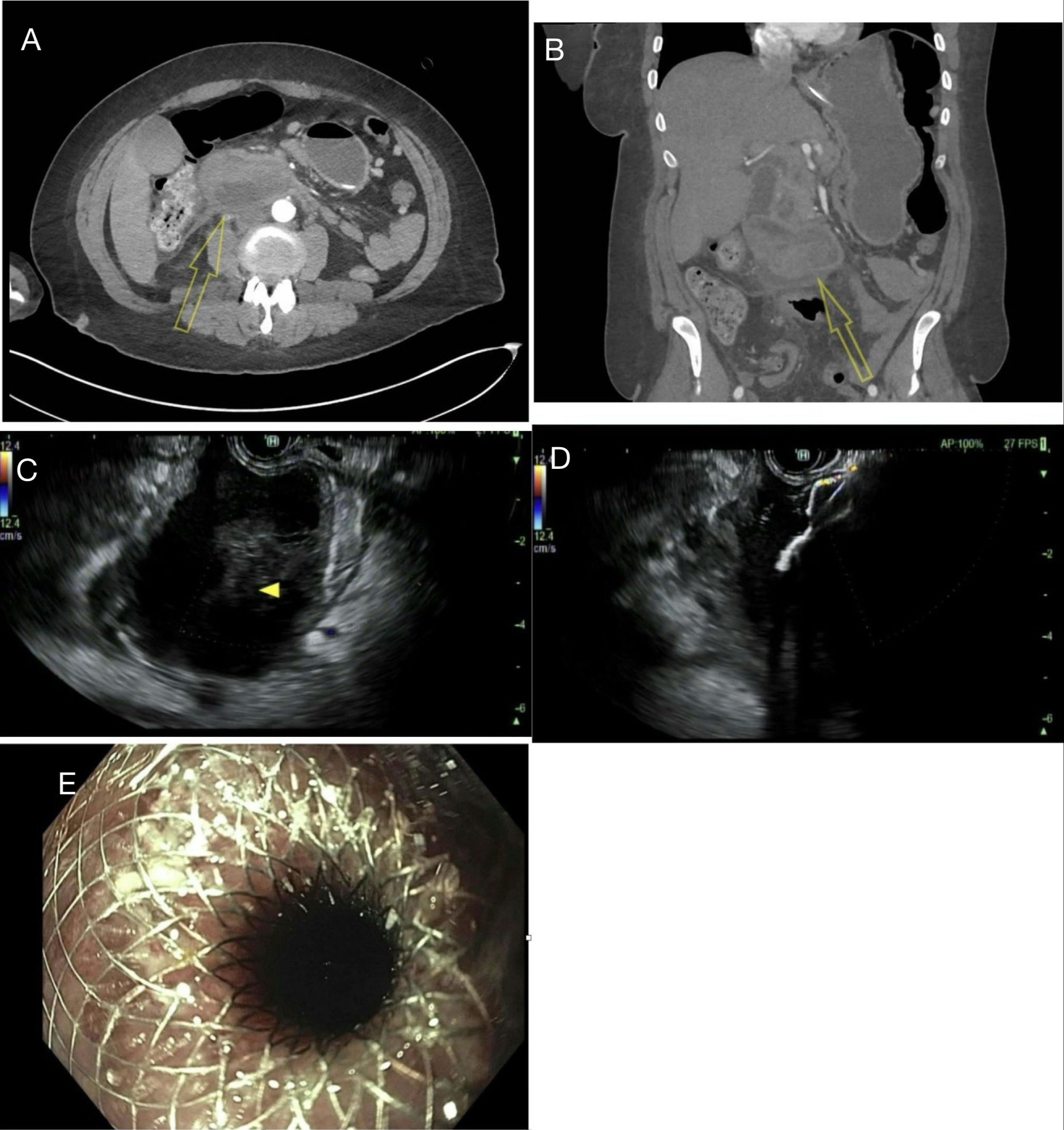
Figure: Picture A and B, arrows pointing toward duodenal hematoma; Picture C is EUS view of the duodenal hematoma ; Picture D deployment of the stent; Picture E showing the stent in place
Disclosures:
Mohammed Martini indicated no relevant financial relationships.
Medha Rajamanuri indicated no relevant financial relationships.
Muaataz Azzawi indicated no relevant financial relationships.
Abdul Swied indicated no relevant financial relationships.
Mohammed Martini, MD1, Medha Rajamanuri, MBBS1, Muaataz Azzawi, MD1, Abdul Swied, MD2. P2840 - Endoscopic Drainage of Intramural Duodenal Hematoma Secondary to Acute Pancreatitis Using Lumen-Apposing Metal Stent (LAMS), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
