Monday Poster Session
Category: Liver
P2879 - Combination of Non-Selective Beta Blockers and Statins Is Associated With Decreased 90-Day Mortality in Alcohol-Associated Liver Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- NH
Nariman Hossein-Javaheri, DO
University at Buffalo
Buffalo, NY
Presenting Author(s)
Nariman Hossein-Javaheri, DO1, Blake Podger, DO1, Ikjot Singh, MD1, Himaben Gohil, DO1, Ahmad Abulawi, MD2, Anthony Martinez, MD1
1University at Buffalo, Buffalo, NY; 2Albany Medical Center, Albany, NY
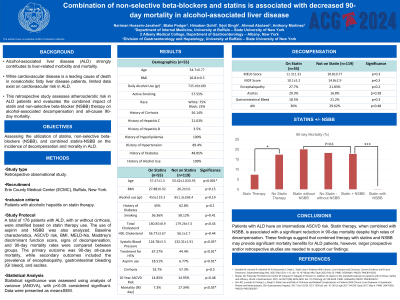
Introduction: Alcohol-associated liver disease (ALD) strongly contributes to liver-related morbidity and mortality. While cardiovascular disease is a leading cause of death in nonalcoholic fatty liver disease patients, limited data exist on cardiovascular risk in ALD. This retrospective study assesses atherosclerotic risk in ALD patients and evaluates the combined impact of statin and non-selective beta-blocker (NSBB) therapy on alcohol-associated decompensation and all-cause 90-day mortality.
Methods: A total of 176 patients with ALD, with or without cirrhosis, were stratified based on statin therapy use. The use of aspirin and NSBB was also analyzed. Baseline characteristics, ASCVD risk, BMI, MELD-Na, Maddrey's discriminant function score, signs of decompensation, and 90-day mortality rates were compared between groups. The primary outcome was 90-day all-cause mortality, while secondary outcomes included the prevalence of encephalopathy, gastrointestinal (GI) bleeding, and ascites. Statistical significance was assessed using analysis of variance (ANOVA), with p< 0.05 considered significant. Data were presented as mean±SEM.
Results: In total, 56.1% had cirrhosis, and 32% were on statin therapy. The average ASCVD risk score was 14.9±1.1. Patients on statins were older (57.4±1.3 vs. 53.4±10.9 years; p< 0.01) and more likely to be on NSBB (67.2% vs. 44.4%; p< 0.01) and aspirin (18.5% vs. 6.7%; p< 0.01). There were no significant differences in BMI (27.8 vs. 26.2; p=0.15), MELD score (11.3±1.3 vs. 10.8±0.4; p=0.3), or Maddrey's discriminant function score (18.2±5.2 vs. 14.8±2.9; p=0.27) between the groups. Rates of encephalopathy (27.7% vs. 21.8%; p=0.2), GI bleed (18.5% vs. 21.1%; p=0.3), and ascites (20.4% vs. 16.8%; p=0.3) were also not significantly different. However, patients on statins had a significantly lower all-cause 90-day mortality rate (7.3% vs. 17.3%; p< 0.05). This mortality benefit persisted among those on NSBB (0% vs. 17.7%; p< 0.01). Notably, statin monotherapy did not demonstrate a significant mortality benefit in patients not taking NSBB (20% vs. 18.2%; p=0.4).
Discussion: Patients with ALD have an intermediate ASCVD risk. Statin therapy, when combined with NSBB, is associated with a significant reduction in 90-day mortality despite high rates of decompensation. These findings suggest that combined therapy with statins and NSBB may provide significant mortality benefits for ALD patients, however, larger prospective and/or retrospective studies are needed to support our findings.
Disclosures:
Nariman Hossein-Javaheri, DO1, Blake Podger, DO1, Ikjot Singh, MD1, Himaben Gohil, DO1, Ahmad Abulawi, MD2, Anthony Martinez, MD1. P2879 - Combination of Non-Selective Beta Blockers and Statins Is Associated With Decreased 90-Day Mortality in Alcohol-Associated Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2Albany Medical Center, Albany, NY
Introduction: Alcohol-associated liver disease (ALD) strongly contributes to liver-related morbidity and mortality. While cardiovascular disease is a leading cause of death in nonalcoholic fatty liver disease patients, limited data exist on cardiovascular risk in ALD. This retrospective study assesses atherosclerotic risk in ALD patients and evaluates the combined impact of statin and non-selective beta-blocker (NSBB) therapy on alcohol-associated decompensation and all-cause 90-day mortality.
Methods: A total of 176 patients with ALD, with or without cirrhosis, were stratified based on statin therapy use. The use of aspirin and NSBB was also analyzed. Baseline characteristics, ASCVD risk, BMI, MELD-Na, Maddrey's discriminant function score, signs of decompensation, and 90-day mortality rates were compared between groups. The primary outcome was 90-day all-cause mortality, while secondary outcomes included the prevalence of encephalopathy, gastrointestinal (GI) bleeding, and ascites. Statistical significance was assessed using analysis of variance (ANOVA), with p< 0.05 considered significant. Data were presented as mean±SEM.
Results: In total, 56.1% had cirrhosis, and 32% were on statin therapy. The average ASCVD risk score was 14.9±1.1. Patients on statins were older (57.4±1.3 vs. 53.4±10.9 years; p< 0.01) and more likely to be on NSBB (67.2% vs. 44.4%; p< 0.01) and aspirin (18.5% vs. 6.7%; p< 0.01). There were no significant differences in BMI (27.8 vs. 26.2; p=0.15), MELD score (11.3±1.3 vs. 10.8±0.4; p=0.3), or Maddrey's discriminant function score (18.2±5.2 vs. 14.8±2.9; p=0.27) between the groups. Rates of encephalopathy (27.7% vs. 21.8%; p=0.2), GI bleed (18.5% vs. 21.1%; p=0.3), and ascites (20.4% vs. 16.8%; p=0.3) were also not significantly different. However, patients on statins had a significantly lower all-cause 90-day mortality rate (7.3% vs. 17.3%; p< 0.05). This mortality benefit persisted among those on NSBB (0% vs. 17.7%; p< 0.01). Notably, statin monotherapy did not demonstrate a significant mortality benefit in patients not taking NSBB (20% vs. 18.2%; p=0.4).
Discussion: Patients with ALD have an intermediate ASCVD risk. Statin therapy, when combined with NSBB, is associated with a significant reduction in 90-day mortality despite high rates of decompensation. These findings suggest that combined therapy with statins and NSBB may provide significant mortality benefits for ALD patients, however, larger prospective and/or retrospective studies are needed to support our findings.
Disclosures:
Nariman Hossein-Javaheri indicated no relevant financial relationships.
Blake Podger indicated no relevant financial relationships.
Ikjot Singh indicated no relevant financial relationships.
Himaben Gohil indicated no relevant financial relationships.
Ahmad Abulawi indicated no relevant financial relationships.
Anthony Martinez: Abbvie – Consultant, Speakers Bureau. Arbutus – Consultant. Braeburn – Speakers Bureau. Gilead – Consultant, Speakers Bureau. Madrigal – Speakers Bureau. Roche – Consultant. Sirtex – Consultant. VBI – Consultant.
Nariman Hossein-Javaheri, DO1, Blake Podger, DO1, Ikjot Singh, MD1, Himaben Gohil, DO1, Ahmad Abulawi, MD2, Anthony Martinez, MD1. P2879 - Combination of Non-Selective Beta Blockers and Statins Is Associated With Decreased 90-Day Mortality in Alcohol-Associated Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
