Tuesday Poster Session
Category: IBD
P4268 - Fecal Microbiota Transplantation for Chronic Pouchitis: An Updated Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Magnus Chun, MD
Kirk Kerkorian School of Medicine at the University of Nevada
Las Vegas, NV
Presenting Author(s)
Magnus Chun, MD1, Kyaw Min Tun, DO1, Tahne Vongsavath, DO2, Kavita Batra, PhD1, David Limsui, MD3, Erin Jenkins, MD4
1Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, NV; 2Kirk Kirkorian School of Medicine, Las Vegas, NV; 3Stanford University School of Medicine, Palo Alto, CA; 4Creighton University School of Medicine, Omaha, NE
Introduction: Pouchitis is a common complication after ileal-pouch anal anastomosis in patients with medically refractory ulcerative colitis. Fecal microbiota transplantation (FMT) has been increasingly studied as a promising therapy to treat chronic pouchitis. However, there has been a lack of high-level evidence and contemporary reviews focusing on its safety and efficacy outcomes. We aim to evaluate multiple outcomes and complications of FMT for treatment of chronic pouchitis.
Methods: PubMed, Embase, Web of Science, CINAHL, Google Scholar, and Cochrane databases were systematically searched to retrieve English-only, original studies, published from inception to March 31, 2024, investigating chronic pouchitis only. Primary outcomes included overall remission, clinical response, clinical remission, clinical relapse, and complications. Secondary outcomes included overall remission and clinical response categorized by donor source and country.
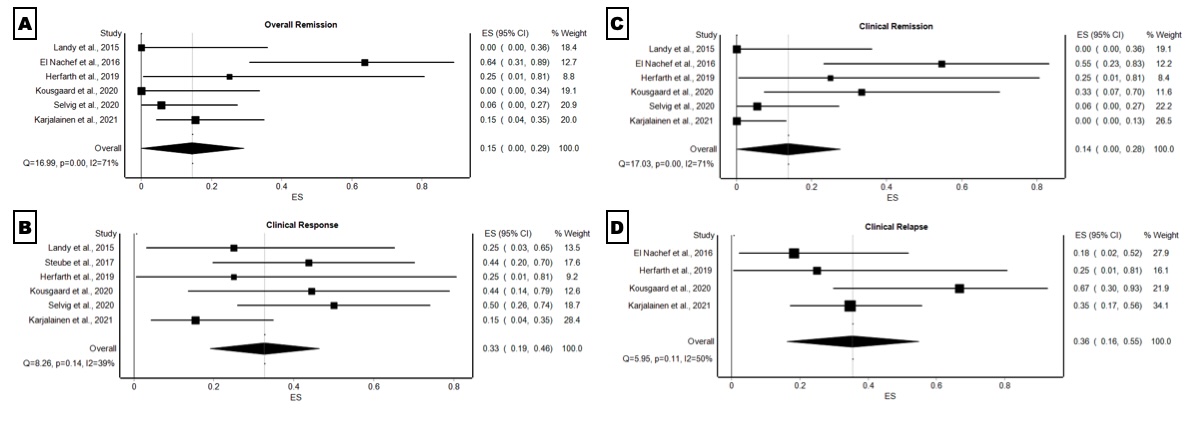
Results: Seven studies with 94 patients receiving FMT were included. Route, preparation, and quantity of FMT administered varied. The pooled overall remission rate (Pouchitis Disease Activity Index score (PDAI) < 7 at 4 weeks follow-up) was 15% (95% CI: 0%-29%, p< 0.001, I2=71%). Additionally, the clinical response rate was 33% (95% CI: 19%-46%, p=0.14, I2=39%), clinical remission rate (PDAI < 4 at 4 weeks follow-up and no need for antibiotics or subjective improvement in symptoms) was 14% (95% CI: 19%-46%, p< 0.001, I2=71%), and the clinical relapse rate was 36% (95% CI: 16%-55%, p=0.11, I2=50%) over the mean follow-up of 29.6 weeks. The pooled proportion of patients with mild adverse events (ASGE severity grading scale) that lasted less than 14 days after FMT treatment was 39% (95% CI: 6%-71%, p< 0.001, I2=94%), with abdominal pain and nausea/vomiting being the most prevalent. No severe adverse events or deaths were reported. FMT with a single donor source had a higher overall remission rate (24%, 95% CI: 2%-46%, p=0.01) compared to multiple donor sources. However, FMT with multiple donor sources had a higher overall clinical response (38%, 95% CI: 22%-55%, p=0.6).
Discussion: Although FMT is an effective treatment for chronic pouchitis, there is still a high rate of mild adverse events. High-level evidence for FMT is still sparse limiting recommendations for its use in clinical practice. Additional trials with greater sample sizes, longer lengths of treatment, to help establish a standardized protocol for FMT therapy in chronic pouchitis would be advantageous.
Disclosures:
Magnus Chun, MD1, Kyaw Min Tun, DO1, Tahne Vongsavath, DO2, Kavita Batra, PhD1, David Limsui, MD3, Erin Jenkins, MD4. P4268 - Fecal Microbiota Transplantation for Chronic Pouchitis: An Updated Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, NV; 2Kirk Kirkorian School of Medicine, Las Vegas, NV; 3Stanford University School of Medicine, Palo Alto, CA; 4Creighton University School of Medicine, Omaha, NE
Introduction: Pouchitis is a common complication after ileal-pouch anal anastomosis in patients with medically refractory ulcerative colitis. Fecal microbiota transplantation (FMT) has been increasingly studied as a promising therapy to treat chronic pouchitis. However, there has been a lack of high-level evidence and contemporary reviews focusing on its safety and efficacy outcomes. We aim to evaluate multiple outcomes and complications of FMT for treatment of chronic pouchitis.
Methods: PubMed, Embase, Web of Science, CINAHL, Google Scholar, and Cochrane databases were systematically searched to retrieve English-only, original studies, published from inception to March 31, 2024, investigating chronic pouchitis only. Primary outcomes included overall remission, clinical response, clinical remission, clinical relapse, and complications. Secondary outcomes included overall remission and clinical response categorized by donor source and country.
Results: Seven studies with 94 patients receiving FMT were included. Route, preparation, and quantity of FMT administered varied. The pooled overall remission rate (Pouchitis Disease Activity Index score (PDAI) < 7 at 4 weeks follow-up) was 15% (95% CI: 0%-29%, p< 0.001, I2=71%). Additionally, the clinical response rate was 33% (95% CI: 19%-46%, p=0.14, I2=39%), clinical remission rate (PDAI < 4 at 4 weeks follow-up and no need for antibiotics or subjective improvement in symptoms) was 14% (95% CI: 19%-46%, p< 0.001, I2=71%), and the clinical relapse rate was 36% (95% CI: 16%-55%, p=0.11, I2=50%) over the mean follow-up of 29.6 weeks. The pooled proportion of patients with mild adverse events (ASGE severity grading scale) that lasted less than 14 days after FMT treatment was 39% (95% CI: 6%-71%, p< 0.001, I2=94%), with abdominal pain and nausea/vomiting being the most prevalent. No severe adverse events or deaths were reported. FMT with a single donor source had a higher overall remission rate (24%, 95% CI: 2%-46%, p=0.01) compared to multiple donor sources. However, FMT with multiple donor sources had a higher overall clinical response (38%, 95% CI: 22%-55%, p=0.6).
Discussion: Although FMT is an effective treatment for chronic pouchitis, there is still a high rate of mild adverse events. High-level evidence for FMT is still sparse limiting recommendations for its use in clinical practice. Additional trials with greater sample sizes, longer lengths of treatment, to help establish a standardized protocol for FMT therapy in chronic pouchitis would be advantageous.
Figure: Figure 1. FMT treatment forest plots of (A) pooled proportion of overall remission, (B) pooled proportion of clinical response, (C) pooled proportion of clinical remission, and (D) pooled proportion of clinical relapse.
Disclosures:
Magnus Chun indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Tahne Vongsavath indicated no relevant financial relationships.
Kavita Batra indicated no relevant financial relationships.
David Limsui indicated no relevant financial relationships.
Erin Jenkins indicated no relevant financial relationships.
Magnus Chun, MD1, Kyaw Min Tun, DO1, Tahne Vongsavath, DO2, Kavita Batra, PhD1, David Limsui, MD3, Erin Jenkins, MD4. P4268 - Fecal Microbiota Transplantation for Chronic Pouchitis: An Updated Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

