Tuesday Poster Session
Category: IBD
P4281 - IBD Patient Preference Study Comparing Monotherapy and Dual Biologic Therapy Among Advanced Therapy Treatment Failures
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ellen M. Janssen, PhD
Janssen Research and Development
Baltimore, MD
Presenting Author(s)
Ellen M. Janssen, PhD1, Anna Sheahan, MSPH, PhD2, John P. Lynch, MD, PhD3, Melissa Marko, PhD4, Meenakshi Bewtra, MD, PhD, MPH5, Matthew J. Wallace, MA6, Jui-Chen Yang, BS7, F. Reed Johnson, PhD8, Laura M Bozzi, PhD9
1Janssen Research and Development, Baltimore, MD; 2Johnson and Johnson, Horsham, PA; 3Johnson & Johnson Innovative Medicine, Springhouse, PA; 4Johnson & Johnson, Spring House, PA; 5University of Pennsylvania, Philadelphia, PA; 6Duke Clinical Research Institute, Beaufort, SC; 7Duke Clinical Research Institute, Bellevue, WA; 8Duke University School of Medicine, Durham, NC; 9Janssen, Raritan, NJ
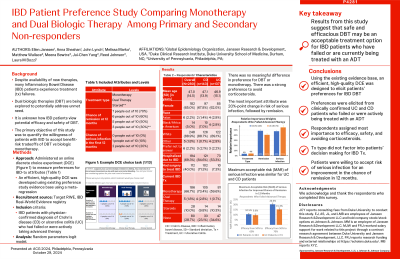
Introduction: Despite availability of new therapies, many patients with Inflammatory Bowel Disease (IBD) still experience treatment failures. Dual biologic therapies are being explored as an option to potentially address this unmet need. It is unknown how IBD patients view potential efficacy and safety risks of dual biologic therapy. The primary objective of this study was to quantify the willingness of patients with IBD to accept benefit-risk tradeoffs related to dual biologic therapy compared to monotherapy.
Methods: Built on the existing IBD treatment-preference studies and evidence base, a discrete choice experiment (DCE) was developed to measure patient preferences for the following treatment characteristics independently: treatment type (dual therapy, monotherapy, or corticosteroids); chance of remission (30%, 50%, 60%, 70%); and risk of serious infection (0%, 10%, 20%). IBD patients with physician-confirmed diagnosis of Crohn’s disease (CD; n=143) or ulcerative colitis (UC; n=137) who had failed or were actively taking advanced therapy were recruited through an IBD registry. DCE responses were analyzed using a random parameters logit model.
Results: Most patients were white, female, had been previously hospitalized for IBD, and were receiving advanced therapies. There was no meaningful difference in preference for dual or monotherapy (p=0.25), while there was strong preference to avoid corticosteroids (p< 0.001), independently of remission and serious infection. A 20-percentage increase in risk of serious infection (53%) was the most important attribute, followed by 20-percentage increase in remission (45%). To improve from 50% to 70% in chance of remission, patients were willing to accept up to 17.5% (95% CI: 17.0%, 18.0%) risk of serious infection. For an improvement in the chance of remission from 50% to 70%, maximum acceptable risk (MAR) among 143 CD patients who had failed therapy was higher than among 74 UC patients who had failed therapy (20.3%, 95% CI:(19.2%, 21.7%) vs. 15.3%, 95% CI:(13.9%, 16.6%)). To improve chance of remission from 50% to 60%, MAR was similar among CD and UC patients.
Discussion: Patients were willing to accept a considerable amount of risk of serious infection for an improvement in the chance of remission at 12 months. Treatment type was not a key driver in patients’ treatment decision making. These results suggest that safe and efficacious dual biologic therapy may be an acceptable treatment option for IBD patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ellen M. Janssen, PhD1, Anna Sheahan, MSPH, PhD2, John P. Lynch, MD, PhD3, Melissa Marko, PhD4, Meenakshi Bewtra, MD, PhD, MPH5, Matthew J. Wallace, MA6, Jui-Chen Yang, BS7, F. Reed Johnson, PhD8, Laura M Bozzi, PhD9. P4281 - IBD Patient Preference Study Comparing Monotherapy and Dual Biologic Therapy Among Advanced Therapy Treatment Failures, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Janssen Research and Development, Baltimore, MD; 2Johnson and Johnson, Horsham, PA; 3Johnson & Johnson Innovative Medicine, Springhouse, PA; 4Johnson & Johnson, Spring House, PA; 5University of Pennsylvania, Philadelphia, PA; 6Duke Clinical Research Institute, Beaufort, SC; 7Duke Clinical Research Institute, Bellevue, WA; 8Duke University School of Medicine, Durham, NC; 9Janssen, Raritan, NJ
Introduction: Despite availability of new therapies, many patients with Inflammatory Bowel Disease (IBD) still experience treatment failures. Dual biologic therapies are being explored as an option to potentially address this unmet need. It is unknown how IBD patients view potential efficacy and safety risks of dual biologic therapy. The primary objective of this study was to quantify the willingness of patients with IBD to accept benefit-risk tradeoffs related to dual biologic therapy compared to monotherapy.
Methods: Built on the existing IBD treatment-preference studies and evidence base, a discrete choice experiment (DCE) was developed to measure patient preferences for the following treatment characteristics independently: treatment type (dual therapy, monotherapy, or corticosteroids); chance of remission (30%, 50%, 60%, 70%); and risk of serious infection (0%, 10%, 20%). IBD patients with physician-confirmed diagnosis of Crohn’s disease (CD; n=143) or ulcerative colitis (UC; n=137) who had failed or were actively taking advanced therapy were recruited through an IBD registry. DCE responses were analyzed using a random parameters logit model.
Results: Most patients were white, female, had been previously hospitalized for IBD, and were receiving advanced therapies. There was no meaningful difference in preference for dual or monotherapy (p=0.25), while there was strong preference to avoid corticosteroids (p< 0.001), independently of remission and serious infection. A 20-percentage increase in risk of serious infection (53%) was the most important attribute, followed by 20-percentage increase in remission (45%). To improve from 50% to 70% in chance of remission, patients were willing to accept up to 17.5% (95% CI: 17.0%, 18.0%) risk of serious infection. For an improvement in the chance of remission from 50% to 70%, maximum acceptable risk (MAR) among 143 CD patients who had failed therapy was higher than among 74 UC patients who had failed therapy (20.3%, 95% CI:(19.2%, 21.7%) vs. 15.3%, 95% CI:(13.9%, 16.6%)). To improve chance of remission from 50% to 60%, MAR was similar among CD and UC patients.
Discussion: Patients were willing to accept a considerable amount of risk of serious infection for an improvement in the chance of remission at 12 months. Treatment type was not a key driver in patients’ treatment decision making. These results suggest that safe and efficacious dual biologic therapy may be an acceptable treatment option for IBD patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ellen Janssen: Johnson & Johnson – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Anna Sheahan: Johnson and Johnson – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds). UCB – Stock-publicly held company(excluding mutual/index funds).
John Lynch: Johnson & Johnson – Employee.
Melissa Marko indicated no relevant financial relationships.
Meenakshi Bewtra: Iterative Health – Grant/Research Support. Johnson & Johnson – Grant/Research Support. MedEd Consultant – Speakers Bureau. Pfizer – Advisory Committee/Board Member.
Matthew Wallace indicated no relevant financial relationships.
Jui-Chen Yang indicated no relevant financial relationships.
F. Reed Johnson: Abbott – Grant/Research Support. Janssen – Grant/Research Support. Merck – Grant/Research Support. Pfizer – Grant/Research Support. Takeda – Grant/Research Support.
Laura M Bozzi: Janssen – Employee, Stock Options.
Ellen M. Janssen, PhD1, Anna Sheahan, MSPH, PhD2, John P. Lynch, MD, PhD3, Melissa Marko, PhD4, Meenakshi Bewtra, MD, PhD, MPH5, Matthew J. Wallace, MA6, Jui-Chen Yang, BS7, F. Reed Johnson, PhD8, Laura M Bozzi, PhD9. P4281 - IBD Patient Preference Study Comparing Monotherapy and Dual Biologic Therapy Among Advanced Therapy Treatment Failures, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
