Tuesday Poster Session
Category: IBD
P4283 - Corticosteroids Prior to Antimicrobials Do Not Increase the Risk of Adverse Outcomes Among Individuals Hospitalized for IBD Flares Complicated by Enteric Pathogens
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SM
Sophie Montgomery, BA, MD
NYU Grossman School of Medicine
Brookline, MA
Presenting Author(s)
Sophie Montgomery, BA, MD1, Jordan Axelrad, MD, MPH2, Olivia R. Delau, MS3, Aasma Shaukat, MD, MPH4, Adam S.. Faye, MD2
1NYU Grossman School of Medicine, Brookline, MA; 2NYU Grossman School of Medicine, New York, NY; 3NYU Langone Health Inflammatory Bowel Disease Center, Cortlandt Manor, NY; 4NYU Langone Health, New York, NY
Introduction: Corticosteroids (CS) are often necessary to treat individuals hospitalized with inflammatory bowel disease (IBD), however there is concern that CS use prior to antimicrobial (AM) therapy among individuals with a concomitant gastrointestinal infection may worsen outcomes. The aim of this study was to explore this.
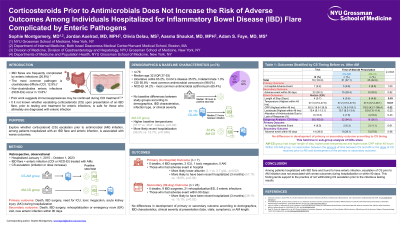
Methods: This was a retrospective study of patients ≥18 years-old who were hospitalized for an IBD flare between 2015-2023. Individuals found to have an enteric infection requiring both CS and AM were included and divided into two groups: those who received CS initiation or escalation prior to (CS-AM) or after (AM-CS) AM therapy initiation. The primary outcome was a composite of death, IBD-related surgery, need for ICU, toxic megacolon, or acute kidney injury during hospitalization. The secondary outcome was a composite of death, IBD-related surgery, rehospitalization or emergency room visit, or subsequent enteric infection within 90 days from presentation.
Results: A total of 76 patients were included; 48 with ulcerative colitis (63.2%), 27 with Crohn’s disease (35.5%), and 1 with indeterminate colitis (1.3%); of whom 50 had Clostridioides difficile (CDI; 65.8%). The majority of patients (67.1%) received CS prior to AM. Baseline characteristics were similar between groups. On primary analysis, 9.8% of individuals in the CS-AM arm had an adverse outcome as compared to 8.0% in the AM-CS arm (p=1.00). On univariable analysis, those who developed an adverse outcome during hospitalization were more likely to have lower albumin at presentation (3.1 vs. 3.7 g/dL, p=0.02) as well as a recent hospitalization in the preceding 3 months (57.1% vs. 18.8%, p=0.04). When restricting the analysis to patients with CDI, there was no difference between the CS-AM and AM-CS groups in development of the primary (6.3% vs. 11.1%, p=0.61) or secondary outcome (28.1% vs. 27.8%, p=0.98). Notably, the AM-CS group had a longer length of stay (6 vs. 4 days, p=0.03) and longer course of CS after discharge (42 vs. 35 days, p< 0.01).
Discussion: We found that initiation or escalation of CS prior to initiation of AM therapy among individuals hospitalized with an IBD flare complicated by an enteric pathogen did not increase the risk of an adverse in-hospital event or 90-day outcome. Although larger-scale data are needed, our study supports the notion that CS can be safely started among individuals hospitalized for an IBD flare while awaiting results of the gastrointestinal infectious panel.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sophie Montgomery, BA, MD1, Jordan Axelrad, MD, MPH2, Olivia R. Delau, MS3, Aasma Shaukat, MD, MPH4, Adam S.. Faye, MD2. P4283 - Corticosteroids Prior to Antimicrobials Do Not Increase the Risk of Adverse Outcomes Among Individuals Hospitalized for IBD Flares Complicated by Enteric Pathogens, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYU Grossman School of Medicine, Brookline, MA; 2NYU Grossman School of Medicine, New York, NY; 3NYU Langone Health Inflammatory Bowel Disease Center, Cortlandt Manor, NY; 4NYU Langone Health, New York, NY
Introduction: Corticosteroids (CS) are often necessary to treat individuals hospitalized with inflammatory bowel disease (IBD), however there is concern that CS use prior to antimicrobial (AM) therapy among individuals with a concomitant gastrointestinal infection may worsen outcomes. The aim of this study was to explore this.
Methods: This was a retrospective study of patients ≥18 years-old who were hospitalized for an IBD flare between 2015-2023. Individuals found to have an enteric infection requiring both CS and AM were included and divided into two groups: those who received CS initiation or escalation prior to (CS-AM) or after (AM-CS) AM therapy initiation. The primary outcome was a composite of death, IBD-related surgery, need for ICU, toxic megacolon, or acute kidney injury during hospitalization. The secondary outcome was a composite of death, IBD-related surgery, rehospitalization or emergency room visit, or subsequent enteric infection within 90 days from presentation.
Results: A total of 76 patients were included; 48 with ulcerative colitis (63.2%), 27 with Crohn’s disease (35.5%), and 1 with indeterminate colitis (1.3%); of whom 50 had Clostridioides difficile (CDI; 65.8%). The majority of patients (67.1%) received CS prior to AM. Baseline characteristics were similar between groups. On primary analysis, 9.8% of individuals in the CS-AM arm had an adverse outcome as compared to 8.0% in the AM-CS arm (p=1.00). On univariable analysis, those who developed an adverse outcome during hospitalization were more likely to have lower albumin at presentation (3.1 vs. 3.7 g/dL, p=0.02) as well as a recent hospitalization in the preceding 3 months (57.1% vs. 18.8%, p=0.04). When restricting the analysis to patients with CDI, there was no difference between the CS-AM and AM-CS groups in development of the primary (6.3% vs. 11.1%, p=0.61) or secondary outcome (28.1% vs. 27.8%, p=0.98). Notably, the AM-CS group had a longer length of stay (6 vs. 4 days, p=0.03) and longer course of CS after discharge (42 vs. 35 days, p< 0.01).
Discussion: We found that initiation or escalation of CS prior to initiation of AM therapy among individuals hospitalized with an IBD flare complicated by an enteric pathogen did not increase the risk of an adverse in-hospital event or 90-day outcome. Although larger-scale data are needed, our study supports the notion that CS can be safely started among individuals hospitalized for an IBD flare while awaiting results of the gastrointestinal infectious panel.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sophie Montgomery indicated no relevant financial relationships.
Jordan Axelrad: Abbvie – Consultant. Adiso – Consultant. Biomerieux – Consultant. BMS – Consultant. Fresenius – Consultant. Genentech – Grant/Research Support. Janssen – Consultant. Pfizer – Consultant.
Olivia Delau indicated no relevant financial relationships.
Aasma Shaukat: iterative health; Freenome – Consultant.
Adam Faye: Abbvie – Consultant. BMS – Consultant. Takeda – Education Seminar.
Sophie Montgomery, BA, MD1, Jordan Axelrad, MD, MPH2, Olivia R. Delau, MS3, Aasma Shaukat, MD, MPH4, Adam S.. Faye, MD2. P4283 - Corticosteroids Prior to Antimicrobials Do Not Increase the Risk of Adverse Outcomes Among Individuals Hospitalized for IBD Flares Complicated by Enteric Pathogens, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

