Tuesday Poster Session
Category: IBD
P4284 - The Impact of Malnutrition on Cardiovascular Outcomes of Hospitalized Patients With Inflammatory Bowel Disease (IBD) in the United States
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Kibwey Peterkin, MD
One Brooklyn Health-Brookdale University Hospital Medical Center
Brooklyn, NY
Presenting Author(s)
Kibwey Peterkin, MD1, Carina-Leigh Lezama, MD2, Shani Mc Lean, MD1, Abiolah Telesford, MD1, Jamal Perry, MD1, Ifeanyi Uche, MD1, Chidiebele Emmanuel Omaliko, MD1, Chukwuka Eneh, MD1, Oluwasegun Matthew Akinti, MD1, Ayomide Gbenle, MD1
1One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 2Peterborough City Hospital, Peterborough, England, United Kingdom
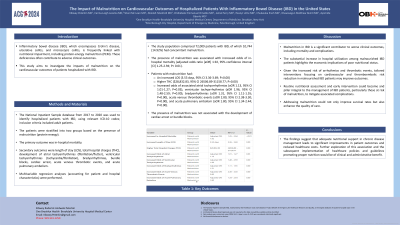
Introduction: Inflammatory bowel disease (IBD), encompassing Crohn's disease, ulcerative colitis, and microscopic colitis, is frequently linked to nutritional impairments, including protein-energy malnutrition (PEM). These nutritional deficits often contribute to adverse clinical outcomes. This study aims to investigate the impacts of malnutrition on the cardiovascular outcomes of patients hospitalized with IBD.
Methods: The National Inpatient Sample database from 2017 to 2020 was used to identify hospitalized patients with IBD, using relevant ICD-10 codes; inclusion criteria included adult patients. The patients were stratified into two groups based on the presence of malnutrition (protein-energy). The primary outcome was in-hospital mortality. Secondary outcomes were length of stay (LOS), total hospital charges (THC), development of atrial tachyarrhythmias (fibrillation/flutter), ventricular tachyarrhythmias (tachycardia/fibrillation), bradyarrhythmias, bundle blocks, cardiac arrest, acute venous thrombotic events, and acute pulmonary embolism. Multivariable regression analyses (accounting for patient and hospital characteristics) were performed.
Results: The study population comprised 72,009 patients with IBD, of which 10,744 (14.92%) had concomitant malnutrition. On multivariate analysis, the presence of malnutrition was associated with increased odds of in-hospital mortality (adjusted odds ratio [aOR] 1.92, 95% confidence interval [CI] 1.25-2.94; P< 0.01). Patients with malnutrition had an increased LOS (3.53 days, 95% CI 3.36-3.69; P=0.00), higher THC ($28,832.83, 95% CI 26506.89-31158.77; P=0.00), increased odds developing atrial tachyarrhythmias (aOR 1.13, 95% CI 1.01-1.27; P=0.03), ventricular tachyarrhythmias (aOR 1.96, 95% CI 1.48-2.59; P=0.00), bradyarrhythmias (aOR 1.31, 95% CI 1.11-1.55; P=0.00), acute venous thrombotic events (aOR 2.80, 95% CI 2.38-3.30; P=0.00), and acute pulmonary embolism (aOR 1.80, 95% CI 1.34-2.44; P=0.00).The presence of malnutrition was not associated with the development of cardiac arrest or bundle blocks.
Discussion: Malnutrition negatively impacts in-hospital mortality and increased healthcare resource utilization, including longer hospital stays, higher hospital charges, and increased odds of developing atrial tachyarrhythmias, ventricular tachyarrhythmias, bradyarrhythmias, acute venous thrombotic events, and acute pulmonary embolism. These findings highlight the critical impact of malnutrition on clinical outcomes and healthcare utilization in IBD patients.
Disclosures:
Kibwey Peterkin, MD1, Carina-Leigh Lezama, MD2, Shani Mc Lean, MD1, Abiolah Telesford, MD1, Jamal Perry, MD1, Ifeanyi Uche, MD1, Chidiebele Emmanuel Omaliko, MD1, Chukwuka Eneh, MD1, Oluwasegun Matthew Akinti, MD1, Ayomide Gbenle, MD1. P4284 - The Impact of Malnutrition on Cardiovascular Outcomes of Hospitalized Patients With Inflammatory Bowel Disease (IBD) in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 2Peterborough City Hospital, Peterborough, England, United Kingdom
Introduction: Inflammatory bowel disease (IBD), encompassing Crohn's disease, ulcerative colitis, and microscopic colitis, is frequently linked to nutritional impairments, including protein-energy malnutrition (PEM). These nutritional deficits often contribute to adverse clinical outcomes. This study aims to investigate the impacts of malnutrition on the cardiovascular outcomes of patients hospitalized with IBD.
Methods: The National Inpatient Sample database from 2017 to 2020 was used to identify hospitalized patients with IBD, using relevant ICD-10 codes; inclusion criteria included adult patients. The patients were stratified into two groups based on the presence of malnutrition (protein-energy). The primary outcome was in-hospital mortality. Secondary outcomes were length of stay (LOS), total hospital charges (THC), development of atrial tachyarrhythmias (fibrillation/flutter), ventricular tachyarrhythmias (tachycardia/fibrillation), bradyarrhythmias, bundle blocks, cardiac arrest, acute venous thrombotic events, and acute pulmonary embolism. Multivariable regression analyses (accounting for patient and hospital characteristics) were performed.
Results: The study population comprised 72,009 patients with IBD, of which 10,744 (14.92%) had concomitant malnutrition. On multivariate analysis, the presence of malnutrition was associated with increased odds of in-hospital mortality (adjusted odds ratio [aOR] 1.92, 95% confidence interval [CI] 1.25-2.94; P< 0.01). Patients with malnutrition had an increased LOS (3.53 days, 95% CI 3.36-3.69; P=0.00), higher THC ($28,832.83, 95% CI 26506.89-31158.77; P=0.00), increased odds developing atrial tachyarrhythmias (aOR 1.13, 95% CI 1.01-1.27; P=0.03), ventricular tachyarrhythmias (aOR 1.96, 95% CI 1.48-2.59; P=0.00), bradyarrhythmias (aOR 1.31, 95% CI 1.11-1.55; P=0.00), acute venous thrombotic events (aOR 2.80, 95% CI 2.38-3.30; P=0.00), and acute pulmonary embolism (aOR 1.80, 95% CI 1.34-2.44; P=0.00).The presence of malnutrition was not associated with the development of cardiac arrest or bundle blocks.
Discussion: Malnutrition negatively impacts in-hospital mortality and increased healthcare resource utilization, including longer hospital stays, higher hospital charges, and increased odds of developing atrial tachyarrhythmias, ventricular tachyarrhythmias, bradyarrhythmias, acute venous thrombotic events, and acute pulmonary embolism. These findings highlight the critical impact of malnutrition on clinical outcomes and healthcare utilization in IBD patients.
Disclosures:
Kibwey Peterkin indicated no relevant financial relationships.
Carina-Leigh Lezama indicated no relevant financial relationships.
Shani Mc Lean indicated no relevant financial relationships.
Abiolah Telesford indicated no relevant financial relationships.
Jamal Perry indicated no relevant financial relationships.
Ifeanyi Uche indicated no relevant financial relationships.
Chidiebele Emmanuel Omaliko indicated no relevant financial relationships.
Chukwuka Eneh indicated no relevant financial relationships.
Oluwasegun Matthew Akinti indicated no relevant financial relationships.
Ayomide Gbenle indicated no relevant financial relationships.
Kibwey Peterkin, MD1, Carina-Leigh Lezama, MD2, Shani Mc Lean, MD1, Abiolah Telesford, MD1, Jamal Perry, MD1, Ifeanyi Uche, MD1, Chidiebele Emmanuel Omaliko, MD1, Chukwuka Eneh, MD1, Oluwasegun Matthew Akinti, MD1, Ayomide Gbenle, MD1. P4284 - The Impact of Malnutrition on Cardiovascular Outcomes of Hospitalized Patients With Inflammatory Bowel Disease (IBD) in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

