Tuesday Poster Session
Category: IBD
P4293 - Comparative Outcomes of Laparoscopic vs Open IPAA in Patients With IBD: A Propensity Score-Matched Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- TK
Tushar Khanna, MD
Penn Medicine
Philadelphia, PA
Presenting Author(s)
Tushar Khanna, MD1, Priya Sehgal, MD1, Aakash Desai, MD2, Nilan Nandish, 3, Nahel Tunio, MD4, Gary Lichtenstein, MD1
1Penn Medicine, Philadelphia, PA; 2Mayo Clinic, Pittsburgh, PA; 3University of Pennsylvania, Philadelphia, PA; 4Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction: Laparoscopic ileal pouch-anal anastomosis (IPAA) has been gaining popularity due to its minimally invasive approach, and association with shorter hospitalization and quicker return of bowel function. It is, however, also associated with a longer operative time. There is limited large scale, population level data comparing post-operative pouch-related complications between laparoscopic and open technique. Our study aims to compare long term postoperative outcomes of laparoscopic versus open IPAA in IBD patients using propensity score matching from a large, nationally representative database.
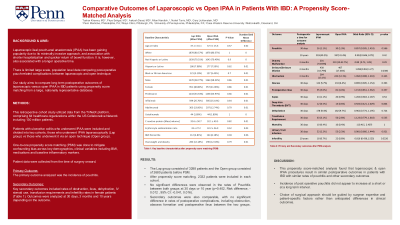
Methods: This retrospective cohort study utilized data from the TriNetX platform, comprising 64 healthcare organizations within the US Collaborative Network including 130 million patients. Patients with ulcerative colitis who underwent IPAA were included and divided into two cohorts, those who underwent IPAA laparoscopically (Lap group) vs those who underwent it via an open technique (Open group). One-to-one propensity score matching (PSM) was done to mitigate confounding bias across key demographics, clinical variables including BMI, medications and baseline inflammatory markers. Patient data were collected from the time of surgery onward. The primary outcome analyzed was the incidence of pouchitis. Key secondary outcomes included rates of obstruction, ileus, dehydration, IV steroid use, transfusion requirements and infertility rates in female patients (Table 1). Outcomes were analyzed at 30 days, 3 months and 10 years depending on the outcome.
Results: The Lap group consisted of 3288 patients and the Open group consisted of 2680 patients before PSM. After propensity score matching, 2332 patients were included in each cohort. No significant differences were observed in the rates of Pouchitis between both groups at 30 days or 10 year (p=0.402, Risk difference, -0.012 , 95% CI: -0.041, 0.016). Secondary outcomes were also comparable, with no significant difference in rates of postoperative complications, including obstruction, abscess formation and postoperative ileus between the two groups.
Discussion: This propensity score-matched analysis found that laparoscopic & open IPAA procedures result in similar postoperative outcomes in patients with IBD. Therefore, the choice of surgical approach should be guided by surgeon expertise and patient-specific factors rather than anticipated differences in clinical outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tushar Khanna, MD1, Priya Sehgal, MD1, Aakash Desai, MD2, Nilan Nandish, 3, Nahel Tunio, MD4, Gary Lichtenstein, MD1. P4293 - Comparative Outcomes of Laparoscopic vs Open IPAA in Patients With IBD: A Propensity Score-Matched Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Penn Medicine, Philadelphia, PA; 2Mayo Clinic, Pittsburgh, PA; 3University of Pennsylvania, Philadelphia, PA; 4Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction: Laparoscopic ileal pouch-anal anastomosis (IPAA) has been gaining popularity due to its minimally invasive approach, and association with shorter hospitalization and quicker return of bowel function. It is, however, also associated with a longer operative time. There is limited large scale, population level data comparing post-operative pouch-related complications between laparoscopic and open technique. Our study aims to compare long term postoperative outcomes of laparoscopic versus open IPAA in IBD patients using propensity score matching from a large, nationally representative database.
Methods: This retrospective cohort study utilized data from the TriNetX platform, comprising 64 healthcare organizations within the US Collaborative Network including 130 million patients. Patients with ulcerative colitis who underwent IPAA were included and divided into two cohorts, those who underwent IPAA laparoscopically (Lap group) vs those who underwent it via an open technique (Open group). One-to-one propensity score matching (PSM) was done to mitigate confounding bias across key demographics, clinical variables including BMI, medications and baseline inflammatory markers. Patient data were collected from the time of surgery onward. The primary outcome analyzed was the incidence of pouchitis. Key secondary outcomes included rates of obstruction, ileus, dehydration, IV steroid use, transfusion requirements and infertility rates in female patients (Table 1). Outcomes were analyzed at 30 days, 3 months and 10 years depending on the outcome.
Results: The Lap group consisted of 3288 patients and the Open group consisted of 2680 patients before PSM. After propensity score matching, 2332 patients were included in each cohort. No significant differences were observed in the rates of Pouchitis between both groups at 30 days or 10 year (p=0.402, Risk difference, -0.012 , 95% CI: -0.041, 0.016). Secondary outcomes were also comparable, with no significant difference in rates of postoperative complications, including obstruction, abscess formation and postoperative ileus between the two groups.
Discussion: This propensity score-matched analysis found that laparoscopic & open IPAA procedures result in similar postoperative outcomes in patients with IBD. Therefore, the choice of surgical approach should be guided by surgeon expertise and patient-specific factors rather than anticipated differences in clinical outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tushar Khanna indicated no relevant financial relationships.
Priya Sehgal indicated no relevant financial relationships.
Aakash Desai indicated no relevant financial relationships.
Nilan Nandish indicated no relevant financial relationships.
Nahel Tunio indicated no relevant financial relationships.
Gary Lichtenstein indicated no relevant financial relationships.
Tushar Khanna, MD1, Priya Sehgal, MD1, Aakash Desai, MD2, Nilan Nandish, 3, Nahel Tunio, MD4, Gary Lichtenstein, MD1. P4293 - Comparative Outcomes of Laparoscopic vs Open IPAA in Patients With IBD: A Propensity Score-Matched Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
