Tuesday Poster Session
Category: IBD
P4295 - Outcomes of Patients With Inflammatory Bowel Disease on GLP-1 Receptor Agonists: A Propensity Score-Matched Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- TK
Tushar Khanna, MD
Penn Medicine
Philadelphia, PA
Presenting Author(s)
Tushar Khanna, MD1, Priya Sehgal, MD, MS, MPH2, Aakash Desai, MD3, Nahel Tunio, MD4, Emad Mansoor, MD5, Gary Lichtenstein, MD1
1Penn Medicine, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA; 3Mayo Clinic, Pittsburgh, PA; 4Case Western Reserve University / MetroHealth, Cleveland, OH; 5Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: GLP-1 receptor agonists (GLP-1RA) have a demonstrated efficacy in managing T2DM as well as obesity. However, the impact of GLP-1RA on patients with Inflammatory Bowel Disease (IBD) remains unclear. This study aims to evaluate IBD-related outcomes in patients treated with GLP-1RA using a large nationally representative population.
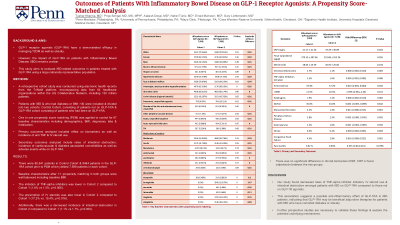
Methods: A retrospective cohort study was conducted using electronic health records from the TriNetX platform, encompassing data from 64 healthcare organizations within the US Collaborative Network, including 130 million patients. Patients with IBD & who had diabetes or BMI >30 were included & divided into two cohorts: Control Cohort, consisting of patients not on GLP-1RA & GLP-1RA cohort consisting of patients who had been on GLP-1RA. One to one propensity score matching (PSM) was applied to control for 67 baseline characteristics including demographics, BMI, diagnoses, labs & medication. Primary outcomes analyzed included effect on biomarkers as well as incidence of anti TNF & IV steroid use. Secondary outcomes analyzed include rates of intestinal obstruction, incidence of cardiovascular & diabetes associated comorbidities as well as adverse events while on GLP-1RA. (Table 1)
Results: There were 80,541 patients in Control Cohort & 8484 patients in the GLP-1RA cohort prior to PSM which yielded 7,599 patients in each cohort. Baseline characteristics after 1:1 propensity matching in both groups were well balanced including baseline BMI. The initiation of TNF-alpha inhibitors was lower in Cohort 2 compared to Cohort 1 (1.0% vs 1.5%, p=0.006). The prescription of IV steroids was also lower in Cohort 2 compared to Cohort 1 (17.2% vs. 19.4%, p=0.016). Additionally, there was a decreased incidence of intestinal obstruction in Cohort 2 compared to Cohort 1 (1.1% vs 1.7%, p=0.003). There was no significant difference in clinical biomarkers ESR, CRP or fecal calprotectin between the two groups.
Discussion: Our study found decreased rates of TNF-alpha inhibitor initiation, IV steroid use & intestinal obstruction amongst patients with IBD on GLP-1RA compared to those not on GLP-1R agonists. This association suggests a possible anti-inflammatory effect of GLP-1RA in IBD patients, indicating that GLP-1RA may be beneficial adjunctive therapies for patients with IBD who have comorbid diabetes or obesity. Further prospective studies are necessary to validate these findings & explore the potential underlying mechanisms.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tushar Khanna, MD1, Priya Sehgal, MD, MS, MPH2, Aakash Desai, MD3, Nahel Tunio, MD4, Emad Mansoor, MD5, Gary Lichtenstein, MD1. P4295 - Outcomes of Patients With Inflammatory Bowel Disease on GLP-1 Receptor Agonists: A Propensity Score-Matched Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Penn Medicine, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA; 3Mayo Clinic, Pittsburgh, PA; 4Case Western Reserve University / MetroHealth, Cleveland, OH; 5Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: GLP-1 receptor agonists (GLP-1RA) have a demonstrated efficacy in managing T2DM as well as obesity. However, the impact of GLP-1RA on patients with Inflammatory Bowel Disease (IBD) remains unclear. This study aims to evaluate IBD-related outcomes in patients treated with GLP-1RA using a large nationally representative population.
Methods: A retrospective cohort study was conducted using electronic health records from the TriNetX platform, encompassing data from 64 healthcare organizations within the US Collaborative Network, including 130 million patients. Patients with IBD & who had diabetes or BMI >30 were included & divided into two cohorts: Control Cohort, consisting of patients not on GLP-1RA & GLP-1RA cohort consisting of patients who had been on GLP-1RA. One to one propensity score matching (PSM) was applied to control for 67 baseline characteristics including demographics, BMI, diagnoses, labs & medication. Primary outcomes analyzed included effect on biomarkers as well as incidence of anti TNF & IV steroid use. Secondary outcomes analyzed include rates of intestinal obstruction, incidence of cardiovascular & diabetes associated comorbidities as well as adverse events while on GLP-1RA. (Table 1)
Results: There were 80,541 patients in Control Cohort & 8484 patients in the GLP-1RA cohort prior to PSM which yielded 7,599 patients in each cohort. Baseline characteristics after 1:1 propensity matching in both groups were well balanced including baseline BMI. The initiation of TNF-alpha inhibitors was lower in Cohort 2 compared to Cohort 1 (1.0% vs 1.5%, p=0.006). The prescription of IV steroids was also lower in Cohort 2 compared to Cohort 1 (17.2% vs. 19.4%, p=0.016). Additionally, there was a decreased incidence of intestinal obstruction in Cohort 2 compared to Cohort 1 (1.1% vs 1.7%, p=0.003). There was no significant difference in clinical biomarkers ESR, CRP or fecal calprotectin between the two groups.
Discussion: Our study found decreased rates of TNF-alpha inhibitor initiation, IV steroid use & intestinal obstruction amongst patients with IBD on GLP-1RA compared to those not on GLP-1R agonists. This association suggests a possible anti-inflammatory effect of GLP-1RA in IBD patients, indicating that GLP-1RA may be beneficial adjunctive therapies for patients with IBD who have comorbid diabetes or obesity. Further prospective studies are necessary to validate these findings & explore the potential underlying mechanisms.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tushar Khanna indicated no relevant financial relationships.
Priya Sehgal indicated no relevant financial relationships.
Aakash Desai indicated no relevant financial relationships.
Nahel Tunio indicated no relevant financial relationships.
Emad Mansoor: Lilly – Speakers Bureau. Takeda – Speakers Bureau.
Gary Lichtenstein indicated no relevant financial relationships.
Tushar Khanna, MD1, Priya Sehgal, MD, MS, MPH2, Aakash Desai, MD3, Nahel Tunio, MD4, Emad Mansoor, MD5, Gary Lichtenstein, MD1. P4295 - Outcomes of Patients With Inflammatory Bowel Disease on GLP-1 Receptor Agonists: A Propensity Score-Matched Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

