Tuesday Poster Session
Category: IBD
P4302 - Long-Term Efficacy and Safety of Intravenous (IV) Tulisokibart in Patients With Crohn’s Disease (CD): Results from the Open-Label Extension Period of the Phase 2 APOLLO-CD Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Corey A. Siegel, MD, MS
Dartmouth-Hitchcock Medical Center
Lebanon, NH
Presenting Author(s)
Corey A.. Siegel, MD, MS1, Rupert W. Leong, MD, FRACP2, Jaclyn K.. Anderson, DO3, Mark Yen, MD3, Bin Dong, PhD3, Bruce E.. Sands, MD, FACG4, Silvio Danese, MD, PhD5, Brian G.. Feagan, MD6
1Dartmouth-Hitchcock Medical Center, Lebanon, NH; 2Concord Hospital and Macquarie University Hospital, Sydney, New South Wales, Australia; 3Merck & Co., Inc., Rahway, NJ; 4Icahn School of Medicine at Mount Sinai, New York, NY; 5Humanitas Clinical and Research Center - IRCCS, Rozzano and Humanitas University, Pieve Emanuele, Milan, Lombardia, Italy; 6Western University, London, ON, Canada
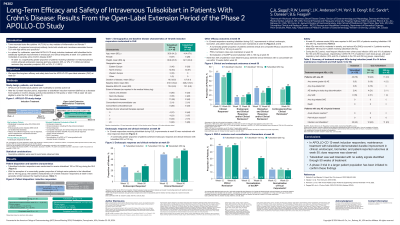
Introduction: Tumor necrosis factor–like cytokine 1A (TL1A) is a mediator of inflammation and fibrosis in CD. Tulisokibart, an anti-TL1A monoclonal antibody, demonstrated robust efficacy without adverse safety signals during the 12-week induction period in adults with moderately to severely active CD in the multicenter, open-label, phase 2a APOLLO-CD study. We report long-term efficacy and safety data for tulisokibart at week 50 from the APOLLO-CD open-label extension (OLE).
Methods: During the 12-week induction period, participants received IV tulisokibart 100 mg on day 1 and 500 mg at weeks 2, 6, and 10. Responders to tulisokibart induction at 12-weeks (defined as a decrease from baseline in CD activity index [CDAI] of ≥100 points or CDAI < 150 at week 12) were given the opportunity to enter the OLE study; 12-week non-responders discontinued the study. At week 14, responders were randomized to receive IV tulisokibart 100 or 250 mg Q4W until week 170. Efficacy outcomes through week 50 in the intention-to-treat population are reported. Safety was evaluated in all participants who received ≥1 dose of tulisokibart. Descriptive statistics were used to summarize observed data.
Results: 53 of 55 participants completed the 12-week induction period; 37 were considered induction responders and were randomized to receive tulisokibart 250 mg (n=18) or 100 mg (n=19). A greater proportion of participants who were biologic-naive entered the OLE in the tulisokibart 250 vs 100 mg group (44% vs 21%). Improvements in clinical, endoscopic, and biomarker outcomes observed with tulisokibart were generally maintained through week 50 in both dose groups. At week 50, a greater proportion of participants achieved clinical and endoscopic outcomes with tulisokibart 250 mg vs 100 mg (Table). Normalization of high-sensitivity C-reactive protein favored the 250 vs the 100 mg dose. At week 50, AEs were reported in 83% and 84% of participants receiving tulisokibart 250 and 100 mg, respectively, and were mostly mild-to-moderate in severity. Serious AEs occurred in 1 (6%) and 2 (11%) participants receiving tulisokibart 250 and 100 mg, respectively.
Discussion: At week 50, maintenance of treatment efficacy was generally observed with tulisokibart in induction responders. A trend for higher maintenance efficacy was observed with tulisokibart 250 vs 100 mg. Tulisokibart was well tolerated with no safety signals identified through 50 weeks of treatment. Larger trials are needed to confirm these findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Corey A.. Siegel, MD, MS1, Rupert W. Leong, MD, FRACP2, Jaclyn K.. Anderson, DO3, Mark Yen, MD3, Bin Dong, PhD3, Bruce E.. Sands, MD, FACG4, Silvio Danese, MD, PhD5, Brian G.. Feagan, MD6. P4302 - Long-Term Efficacy and Safety of Intravenous (IV) Tulisokibart in Patients With Crohn’s Disease (CD): Results from the Open-Label Extension Period of the Phase 2 APOLLO-CD Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Dartmouth-Hitchcock Medical Center, Lebanon, NH; 2Concord Hospital and Macquarie University Hospital, Sydney, New South Wales, Australia; 3Merck & Co., Inc., Rahway, NJ; 4Icahn School of Medicine at Mount Sinai, New York, NY; 5Humanitas Clinical and Research Center - IRCCS, Rozzano and Humanitas University, Pieve Emanuele, Milan, Lombardia, Italy; 6Western University, London, ON, Canada
Introduction: Tumor necrosis factor–like cytokine 1A (TL1A) is a mediator of inflammation and fibrosis in CD. Tulisokibart, an anti-TL1A monoclonal antibody, demonstrated robust efficacy without adverse safety signals during the 12-week induction period in adults with moderately to severely active CD in the multicenter, open-label, phase 2a APOLLO-CD study. We report long-term efficacy and safety data for tulisokibart at week 50 from the APOLLO-CD open-label extension (OLE).
Methods: During the 12-week induction period, participants received IV tulisokibart 100 mg on day 1 and 500 mg at weeks 2, 6, and 10. Responders to tulisokibart induction at 12-weeks (defined as a decrease from baseline in CD activity index [CDAI] of ≥100 points or CDAI < 150 at week 12) were given the opportunity to enter the OLE study; 12-week non-responders discontinued the study. At week 14, responders were randomized to receive IV tulisokibart 100 or 250 mg Q4W until week 170. Efficacy outcomes through week 50 in the intention-to-treat population are reported. Safety was evaluated in all participants who received ≥1 dose of tulisokibart. Descriptive statistics were used to summarize observed data.
Results: 53 of 55 participants completed the 12-week induction period; 37 were considered induction responders and were randomized to receive tulisokibart 250 mg (n=18) or 100 mg (n=19). A greater proportion of participants who were biologic-naive entered the OLE in the tulisokibart 250 vs 100 mg group (44% vs 21%). Improvements in clinical, endoscopic, and biomarker outcomes observed with tulisokibart were generally maintained through week 50 in both dose groups. At week 50, a greater proportion of participants achieved clinical and endoscopic outcomes with tulisokibart 250 mg vs 100 mg (Table). Normalization of high-sensitivity C-reactive protein favored the 250 vs the 100 mg dose. At week 50, AEs were reported in 83% and 84% of participants receiving tulisokibart 250 and 100 mg, respectively, and were mostly mild-to-moderate in severity. Serious AEs occurred in 1 (6%) and 2 (11%) participants receiving tulisokibart 250 and 100 mg, respectively.
Discussion: At week 50, maintenance of treatment efficacy was generally observed with tulisokibart in induction responders. A trend for higher maintenance efficacy was observed with tulisokibart 250 vs 100 mg. Tulisokibart was well tolerated with no safety signals identified through 50 weeks of treatment. Larger trials are needed to confirm these findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Corey Siegel: Abbvie – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker for CME activities. BMS – Advisory Committee/Board Member, Consultant. Boomerang – Advisory Committee/Board Member, Consultant. Buhlman – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker for CME activities. Lilly – Advisory Committee/Board Member, Consultant. Napo pharmaceuticals – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support, speaker for CME activities. Prometheus Biosciences – Advisory Committee/Board Member, Consultant. Prometheus Labs – Advisory Committee/Board Member, Consultant. Roivant – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, speaker for CME activities. Trellus Health – Advisory Committee/Board Member, Consultant.
Rupert W. Leong: Abbvie – Advisory Committee/Board Member. Aspen – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Celgene – Advisory Committee/Board Member. Cellitron – Advisory Committee/Board Member, Grant/Research Support. Chiesi – Advisory Committee/Board Member. Ferring – Advisory Committee/Board Member. Gastroenterological Society of Australia – Grant/Research Support. Glutagen – Advisory Committee/Board Member. Gutsy Group – Grant/Research Support. Hospira – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Grant/Research Support. Joanna Tiddy grant – Grant/Research Support. Lilly – Advisory Committee/Board Member. McKusker Charitable Foundation – Grant/Research Support. MSD – Advisory Committee/Board Member. NHMRC – Grant/Research Support. Novartis – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member, Grant/Research Support. Prometheus Biosciences – Advisory Committee/Board Member. Shire – Grant/Research Support. Takeda – Advisory Committee/Board Member, Grant/Research Support.
Jaclyn Anderson: Merck Sharp & Dohme LLC – Employee.
Mark Yen: Merck Sharp & Dohme LLC – Employee.
Bin Dong: Merck Sharp & Dohme LLC – Employee.
Bruce Sands: AbbVie – Consultant. Abivax – Consultant, Speakers Bureau. Adiso Therapeutics – Consultant. Agomab – Consultant. Alimentiv – Consultant. Amgen – Consultant. AnaptysBio – Consultant. Arena Pharmaceuticals – Consultant. Artugen Therapeutics – Consultant. AstraZeneca – Consultant. Biolojic Design – Consultant. Biora Therapeutics – Consultant. Boehringer Ingelheim – Consultant. Boston Pharmaceuticals – Consultant. Bristol Myers Squibb – Consultant, Grant/Research Support, Other support, Speakers Bureau. Calibr – Consultant. Celgene – Consultant. Celltrion – Consultant. ClostraBio – Consultant. Enthera – Consultant. Envied Biosciences – Consultant. Equilium – Consultant. Evommune – Consultant. Ferring – Consultant. Fiat – Consultant. Fresenius Kabi – Consultant. Galapagos – Consultant. Genentech (Roche) – Consultant. Gilead Sciences – Consultant. Glaxo SmithKline – Consultant. Gossamer Bio – Consultant. Imhotex – Consultant. Index Pharmaceuticals – Consultant. Innovation Pharmaceuticals – Consultant. Inotrem – Consultant. Janssen – Consultant, Grant/Research Support, Other support, Speakers Bureau. Kaleido – Consultant. Kallyope – Consultant. Lilly – Consultant, other support, Speakers Bureau. Merck & Co., Inc., Rahway, NJ, USA – Consultant. Microba – Consultant. Mobius Care – Consultant. Morphic Therapeutics – Consultant. MRM Health – Consultant. Nexus Therapeutics – Consultant. Nimbus Discovery – Consultant. Odyssey Therapeutics – Consultant. Pfizer Inc – Consultant, Grant/Research Support, Other support, Speakers Bureau. Progenity – Consultant. Prometheus Biosciences – Consultant. Prometheus Laboratories – Consultant. Protagonist Therapeutics – Consultant. Q32 Bio – Consultant. Rasayana Therapeutics – Consultant. Recludix Therapeutics – Consultant. Reistone Biopharma – Consultant. Sanofi – Consultant. Spyre Therapeutics – Consultant. Sun Pharma – Consultant. Surrozen – Consultant. Takeda – Consultant, Grant/Research Support, Other support, Speakers Bureau. Target RWE – Consultant. Teva – Consultant. Theravance Biopharma – Consultant, Grant/Research Support. TLL Pharmaceutical – Consultant. Tr1X – Consultant. Union Therapeutics – Consultant. Ventyx Biopharma – Consultant, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Silvio Danese: AbbVie – Consultant, Speakers Bureau. Alimentiv – Consultant. Allergan – Consultant. Amgen – Consultant, Speakers Bureau. Applied Molecular Transport – Consultant. AstraZeneca – Consultant. Athos Therapeutics – Consultant. Biogen – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant. Celgene – Consultant. Celltrion Healthcare – Consultant. Dr Falk Pharma – Consultant. Eli Lilly and Company – Consultant. Enthera – Consultant. Ferring – Consultant, Speakers Bureau. Gilead – Consultant, Speakers Bureau. Hospira – Consultant. Inotrem – Consultant. Janssen – Consultant, Speakers Bureau. Johnson & Johnson – Consultant. Morphic – Consultant. MSD – Consultant. Mundipharma – Consultant. Mylan – Consultant, Speakers Bureau. Pfizer Inc – Consultant, Speakers Bureau. Roche – Consultant. Sandoz – Consultant. Sublimity Therapeutics – Consultant. Takeda – Consultant, Speakers Bureau. Teladoc Health – Consultant. TiGenix – Consultant. UCB Inc. – Consultant. Vial – Consultant. Vifor – Consultant.
Brian Feagan: AbbVie – Advisory Committee/Board Member, Consultant, Speakers Bureau. AbolerIS – Consultant. AgomAB Therapeutics – Consultant. Allianthera – Consultant. Amgen – Advisory Committee/Board Member, Consultant. AnaptysBio – Advisory Committee/Board Member, Consultant. Applied Molecular Transport Inc – Advisory Committee/Board Member, Consultant. Arena Pharma – Consultant. Atomwise – Consultant. Avoro Capital Advisors – Consultant. Axio Research – Advisory Committee/Board Member. BioJamp – Consultant. Biora Therapeutics – Consultant. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant. Boxer – Consultant. Celgene/Bristol Myers Squibb – Advisory Committee/Board Member, Consultant. Celsius Therapeutics – Consultant. Connect BioPharma – Consultant, stock or other ownership interest. Cytoki – Consultant. Disc Medicine – Consultant. Duality – Consultant. EcoR1 Capital – Advisory Committee/Board Member, Consultant. Equillium – Consultant. Ermium – Consultant. First Wave – Consultant. First Word Group – Consultant. Galapagos – Consultant. Galen Atlantica – Consultant. Genentech/Roche – Advisory Committee/Board Member, Consultant. Gilead – Consultant. GlaxoSmithKline – Advisory Committee/Board Member, Consultant. Gossamer Pharma – Consultant, Stock Options. Hinge Bio – Consultant. Hot Spot Therapeutics – Consultant. Imhotex – Consultant. Immunic Therapeutics – Consultant. InDex Pharmaceuticals – Advisory Committee/Board Member, Consultant. JAKAcademy – Consultant. Janssen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Japan Tobacco Inc. – Consultant. Kaleido Biosciences – Consultant. L.E.K. Consulting – Consultant. Landos Biopharma – Consultant. Leadiant – Consultant. Lenczner Slaght – Consultant, payment for expert testimony. LifeSci Capital – Consultant. Lilly – Advisory Committee/Board Member, Consultant. Lument AB – Consultant. Millennium – Consultant. MiroBio – Advisory Committee/Board Member, Consultant. Morgan Lewis – Consultant, payment for expert testimony. Morphic Therapeutics – Advisory Committee/Board Member, Consultant. Mylan – Consultant. OM Pharma – Consultant. Origo BioPharma – Advisory Committee/Board Member, Consultant. Orphagen – Consultant. Pandion Therapeutics – Consultant. Pendopharm – Consultant. Pfizer Inc – Advisory Committee/Board Member, Consultant, Grant/Research Support. Play to Know AG – Consultant. Progenity – Advisory Committee/Board Member, Consultant. Prometheus – Advisory Committee/Board Member, Consultant. Protagonist – Consultant. PTM Therapeutics – Consultant. Q32 Bio – Consultant. Rebiotix – Consultant. REDX – Advisory Committee/Board Member, Consultant. Roche – Consultant. Sandoz – Consultant. Sanofi – Advisory Committee/Board Member, Consultant. Seres Therapeutics – Consultant. Silverback Therapeutics – Consultant. Surrozen Inc. – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Speakers Bureau. Teva – Advisory Committee/Board Member, Consultant. Thelium – Consultant. Tigenix – Consultant. Tillotts Pharma – Advisory Committee/Board Member, Consultant. Ventyx Biosciences – Consultant. VHSquared Ltd – Consultant. Viatris – Consultant. Ysios – Consultant. Ysopia – Consultant. Zealand Pharma – Consultant.
Corey A.. Siegel, MD, MS1, Rupert W. Leong, MD, FRACP2, Jaclyn K.. Anderson, DO3, Mark Yen, MD3, Bin Dong, PhD3, Bruce E.. Sands, MD, FACG4, Silvio Danese, MD, PhD5, Brian G.. Feagan, MD6. P4302 - Long-Term Efficacy and Safety of Intravenous (IV) Tulisokibart in Patients With Crohn’s Disease (CD): Results from the Open-Label Extension Period of the Phase 2 APOLLO-CD Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
