Tuesday Poster Session
Category: IBD
P4312 - Older Adults With Inflammatory Bowel Disease Are at Increased Risk of Dysplasia Progression
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Kate E. Lee, MD, MS
Duke University Medical Center
Durham, NC
Presenting Author(s)
Kate E. Lee, MD, MS1, Anivarya Kumar, BA2, Grace Kim, BS2, Madhura Pande, BS2, Jacqueline M. Emerson, BS2, Maxwell D. Sumner, BS2, Oliver A. Stewart, MD1, Alessandro Racioppi, MS2, Alice A. Agyekum, BS3, Olivia R. Delau, MS4, Aasma Shaukat, MD, MPH5, Jordan Axelrad, MD, MPH6, Chin Hur, MD, MPH3, Bo Shen, MD7, Jane E. Onken, MD, MHS1, Adam S.. Faye, MD6
1Duke University Medical Center, Durham, NC; 2Duke University School of Medicine, Durham, NC; 3Columbia University Irving Medical Center, New York, NY; 4NYU Langone Health Inflammatory Bowel Disease Center, Cortlandt Manor, NY; 5NYU Langone Health, New York, NY; 6NYU Grossman School of Medicine, New York, NY; 7Columbia University, New York, NY
Introduction: Although inflammatory bowel disease (IBD) increases the risk of colorectal cancer (CRC), data detailing which factors increase this risk, as well as the risk of dysplasia progression, are scant in the current biologic-era.
Methods: In a retrospective single-center analysis, we identified 389 patients with ulcerative colitis (UC) or Crohn’s disease (CD) who had at least two colonoscopies between 2008-2024, capturing a colonoscopy for dysplasia surveillance within 5-14 years of IBD diagnosis (“index colonoscopy”) and at least one subsequent colonoscopy. Exclusion criteria included those with primary sclerosing cholangitis, exclusively ileal CD, prior CRC, or a total colectomy prior to index colonoscopy. Univariable analysis assessed risk factors for dysplasia at index colonoscopy (limited N), whereas adjusted Cox proportional hazards models were used to assess dysplasia progression.
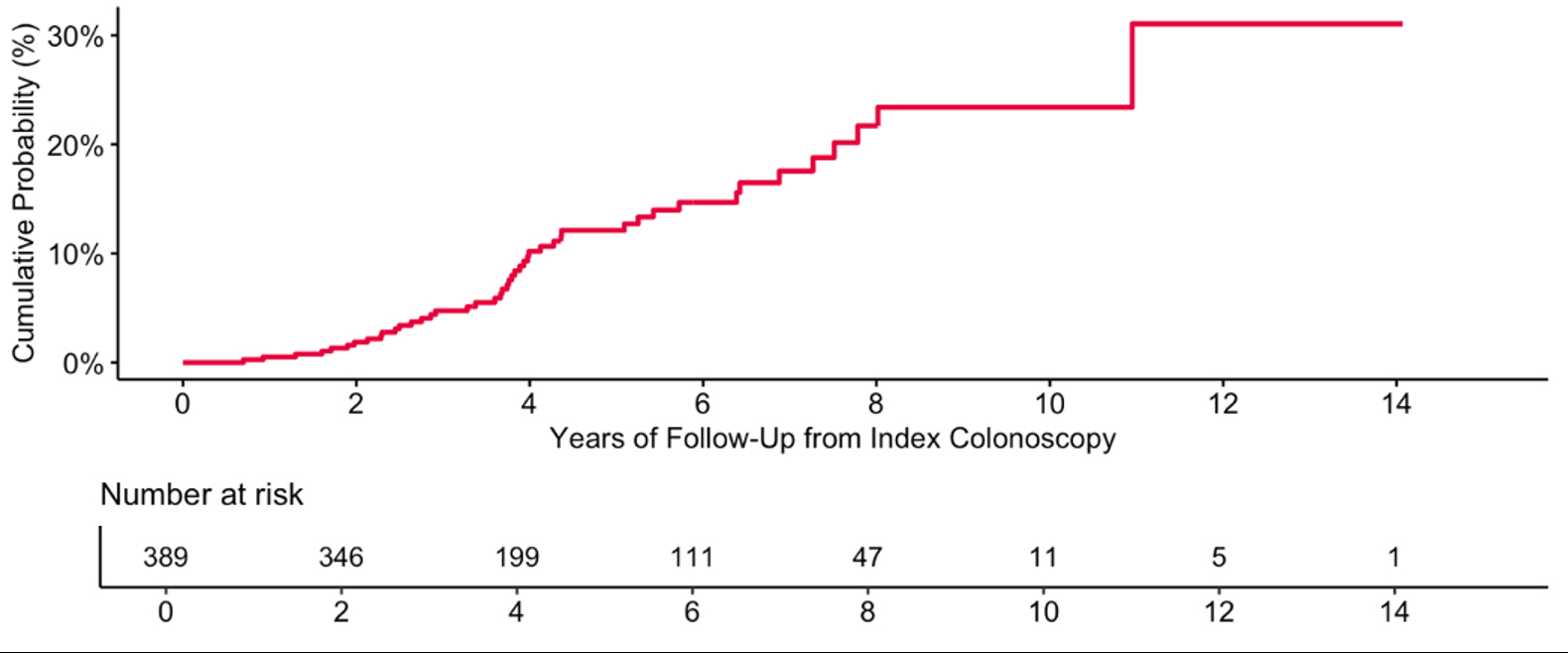
Results: Overall, the median age was 40 years (IQR 29-53 years) with 56.6% female and 52.2% having UC. In total, 24 individuals (6.2%) had low grade dysplasia (LGD) at index colonoscopy, whereas none had high grade dysplasia (HGD)/CRC. On univariable analysis, patients who had dysplasia at index colonoscopy were significantly more likely to be older (58 vs 39 years, p< 0.01), and have had a prior non-CRC related malignancy (p = 0.01). When evaluating dysplasia progression among 389 patients with a median follow-up of 4.1 years (IQR 2.7-6.4) from index colonoscopy, 45 patients initially negative for dysplasia developed LGD (42), HGD (2), or CRC (1) (Figure 1). Further, older age (adjHR 1.04, 95%CI 1.02-1.06) was associated with increased risk of dysplasia progression, even when adjusting for number of colonoscopies (Table 1). On sensitivity analysis, we found similar results when: 1) only including patients with a screening colonoscopy within 8-10 years of IBD diagnosis, 2) ensuring dysplasia was only in areas of remission, and 3) ensuring dysplasia was only in areas of prior known disease activity (to distinguish probable IBD-related dysplasia from sporadic adenoma).
Discussion: Although dysplasia progression was common, HGD and/or CRC were uncommon. Further, we found that older age was associated with the presence of dysplasia at initial surveillance colonoscopy, as well as an independent risk factor for dysplasia progression. Our findings suggest that screening strategies for dysplasia in IBD may need to account for chronological age, though larger-scale studies are needed to confirm this.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kate E. Lee, MD, MS1, Anivarya Kumar, BA2, Grace Kim, BS2, Madhura Pande, BS2, Jacqueline M. Emerson, BS2, Maxwell D. Sumner, BS2, Oliver A. Stewart, MD1, Alessandro Racioppi, MS2, Alice A. Agyekum, BS3, Olivia R. Delau, MS4, Aasma Shaukat, MD, MPH5, Jordan Axelrad, MD, MPH6, Chin Hur, MD, MPH3, Bo Shen, MD7, Jane E. Onken, MD, MHS1, Adam S.. Faye, MD6. P4312 - Older Adults With Inflammatory Bowel Disease Are at Increased Risk of Dysplasia Progression, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Duke University Medical Center, Durham, NC; 2Duke University School of Medicine, Durham, NC; 3Columbia University Irving Medical Center, New York, NY; 4NYU Langone Health Inflammatory Bowel Disease Center, Cortlandt Manor, NY; 5NYU Langone Health, New York, NY; 6NYU Grossman School of Medicine, New York, NY; 7Columbia University, New York, NY
Introduction: Although inflammatory bowel disease (IBD) increases the risk of colorectal cancer (CRC), data detailing which factors increase this risk, as well as the risk of dysplasia progression, are scant in the current biologic-era.
Methods: In a retrospective single-center analysis, we identified 389 patients with ulcerative colitis (UC) or Crohn’s disease (CD) who had at least two colonoscopies between 2008-2024, capturing a colonoscopy for dysplasia surveillance within 5-14 years of IBD diagnosis (“index colonoscopy”) and at least one subsequent colonoscopy. Exclusion criteria included those with primary sclerosing cholangitis, exclusively ileal CD, prior CRC, or a total colectomy prior to index colonoscopy. Univariable analysis assessed risk factors for dysplasia at index colonoscopy (limited N), whereas adjusted Cox proportional hazards models were used to assess dysplasia progression.
Results: Overall, the median age was 40 years (IQR 29-53 years) with 56.6% female and 52.2% having UC. In total, 24 individuals (6.2%) had low grade dysplasia (LGD) at index colonoscopy, whereas none had high grade dysplasia (HGD)/CRC. On univariable analysis, patients who had dysplasia at index colonoscopy were significantly more likely to be older (58 vs 39 years, p< 0.01), and have had a prior non-CRC related malignancy (p = 0.01). When evaluating dysplasia progression among 389 patients with a median follow-up of 4.1 years (IQR 2.7-6.4) from index colonoscopy, 45 patients initially negative for dysplasia developed LGD (42), HGD (2), or CRC (1) (Figure 1). Further, older age (adjHR 1.04, 95%CI 1.02-1.06) was associated with increased risk of dysplasia progression, even when adjusting for number of colonoscopies (Table 1). On sensitivity analysis, we found similar results when: 1) only including patients with a screening colonoscopy within 8-10 years of IBD diagnosis, 2) ensuring dysplasia was only in areas of remission, and 3) ensuring dysplasia was only in areas of prior known disease activity (to distinguish probable IBD-related dysplasia from sporadic adenoma).
Discussion: Although dysplasia progression was common, HGD and/or CRC were uncommon. Further, we found that older age was associated with the presence of dysplasia at initial surveillance colonoscopy, as well as an independent risk factor for dysplasia progression. Our findings suggest that screening strategies for dysplasia in IBD may need to account for chronological age, though larger-scale studies are needed to confirm this.
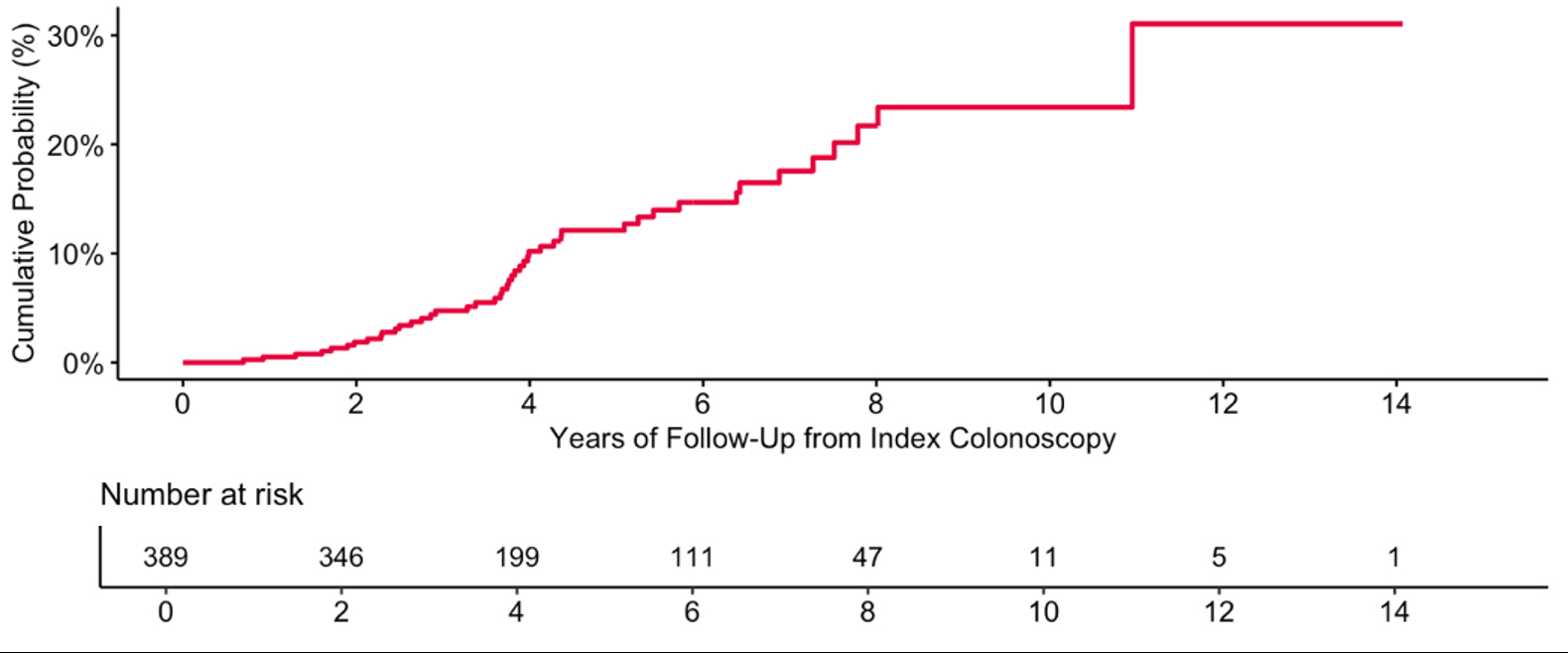
Figure: Figure 1. Cumulative probability of dysplasia (LGD, HGD, CRC) progression.
For patients negative or indefinite for dysplasia at index colonoscopy, follow-up time was calculated to LGD, HGD, or CRC development. For patients with LGD at index colonoscopy, follow-up time was calculated to HGD or CRC progression. Patients without dysplasia development or progression were assessed to latest colonoscopy, unless censored at death or total colectomy. Of 363 patients negative for dysplasia at index colonoscopy, 45 developed LGD, HGD, or CRC at follow-up: 42 patients developed LGD (one of which further progressed to HGD), two patients developed HGD, and one patient developed CRC. Of two patients indefinite for dysplasia at index colonoscopy, none developed LGD, HGD, or CRC. Of 24 patients with LGD at index colonoscopy, none progressed to HGD or CRC.
Abbreviations: LGD (low grade dysplasia), HGD (high grade dysplasia), CRC (colorectal cancer), IBD (inflammatory bowel disease)
For patients negative or indefinite for dysplasia at index colonoscopy, follow-up time was calculated to LGD, HGD, or CRC development. For patients with LGD at index colonoscopy, follow-up time was calculated to HGD or CRC progression. Patients without dysplasia development or progression were assessed to latest colonoscopy, unless censored at death or total colectomy. Of 363 patients negative for dysplasia at index colonoscopy, 45 developed LGD, HGD, or CRC at follow-up: 42 patients developed LGD (one of which further progressed to HGD), two patients developed HGD, and one patient developed CRC. Of two patients indefinite for dysplasia at index colonoscopy, none developed LGD, HGD, or CRC. Of 24 patients with LGD at index colonoscopy, none progressed to HGD or CRC.
Abbreviations: LGD (low grade dysplasia), HGD (high grade dysplasia), CRC (colorectal cancer), IBD (inflammatory bowel disease)
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kate Lee indicated no relevant financial relationships.
Anivarya Kumar indicated no relevant financial relationships.
Grace Kim indicated no relevant financial relationships.
Madhura Pande indicated no relevant financial relationships.
Jacqueline Emerson indicated no relevant financial relationships.
Maxwell Sumner indicated no relevant financial relationships.
Oliver Stewart indicated no relevant financial relationships.
Alessandro Racioppi indicated no relevant financial relationships.
Alice Agyekum indicated no relevant financial relationships.
Olivia Delau indicated no relevant financial relationships.
Aasma Shaukat: iterative health; Freenome – Consultant.
Jordan Axelrad: Abbvie – Consultant. Adiso – Consultant. Biomerieux – Consultant. BMS – Consultant. Fresenius – Consultant. Genentech – Grant/Research Support. Janssen – Consultant. Pfizer – Consultant.
Chin Hur indicated no relevant financial relationships.
Bo Shen indicated no relevant financial relationships.
Jane Onken indicated no relevant financial relationships.
Adam Faye: Abbvie – Consultant. BMS – Consultant. Takeda – Education Seminar.
Kate E. Lee, MD, MS1, Anivarya Kumar, BA2, Grace Kim, BS2, Madhura Pande, BS2, Jacqueline M. Emerson, BS2, Maxwell D. Sumner, BS2, Oliver A. Stewart, MD1, Alessandro Racioppi, MS2, Alice A. Agyekum, BS3, Olivia R. Delau, MS4, Aasma Shaukat, MD, MPH5, Jordan Axelrad, MD, MPH6, Chin Hur, MD, MPH3, Bo Shen, MD7, Jane E. Onken, MD, MHS1, Adam S.. Faye, MD6. P4312 - Older Adults With Inflammatory Bowel Disease Are at Increased Risk of Dysplasia Progression, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
