Tuesday Poster Session
Category: IBD
P4316 - Provider Perceptions and Practices Related to Nutrition Care in Patients with Inflammatory Bowel Disease
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Emily Gore, MD
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Emily Gore, MD, Brijen Shah, MD, Stephanie Gold, MD
Icahn School of Medicine at Mount Sinai, New York, NY
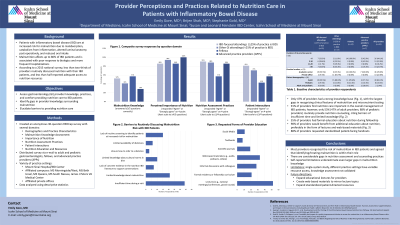
Introduction: Inflammatory bowel disease (IBD) patients are at increased risk for malnutrition due to malabsorption, catabolism from inflammation, altered luminal anatomy post-operatively, and reduced oral intake. According to a 2015 national survey, only 64% of providers routinely discussed nutrition with their IBD patients, and less than half reported adequate access to nutrition resources. We aimed to assess provider knowledge, practices, and comfort providing nutrition care to IBD patients across various groups of providers.
Methods: An anonymous 30-question survey was distributed to adult and pediatric gastroenterologists, fellows, and advanced practice providers (APPs) at an academic medical center and its private affiliates. Questions were organized into several domains, including malnutrition knowledge, perceived importance of nutrition, assessment practices, and education and resources. Data were analyzed using descriptive statistics.
Results: 59 providers completed the survey, including 21(36%) IBD-focused attendings (whose practice is ≥ 25% IBD), 17(29%) attendings with IBD experience (whose practice < 25% IBD), 14(24%) fellows, and 7(12%) APPs. 47% of providers had a strong knowledge base surrounding malnutrition in IBD (answered ≥ 3/5 knowledge-based questions correctly), with the largest gaps in recognizing clinical features of malnutrition and micronutrient testing. 91% of providers found nutrition care important in the overall management of IBD patients and identified their role in assessing nutrition risk. Despite this, 53% of providers (47% of adult providers; 88% of pediatric providers) routinely provide nutrition counseling, citing barriers of insufficient time and limited knowledge. 98% of providers stated they would benefit from additional education about nutrition, preferably in the form of lectures (88%) and web-based materials (56%), with 88% requesting standardized patient-facing handouts.
Discussion: While most providers recognized the risk of malnutrition in IBD patients and agreed that identifying and treating malnutrition is within their role, there were considerable gaps in reported nutrition assessments. Less than half of adult providers routinely offer nutrition counseling due to limited time and knowledge, with self-reported limitations underestimating even larger gaps in malnutrition knowledge. Significant work is needed to improve provider education and expand patient-directed resources to standardize and advance nutrition care for IBD patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Emily Gore, MD, Brijen Shah, MD, Stephanie Gold, MD. P4316 - Provider Perceptions and Practices Related to Nutrition Care in Patients with Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Inflammatory bowel disease (IBD) patients are at increased risk for malnutrition due to malabsorption, catabolism from inflammation, altered luminal anatomy post-operatively, and reduced oral intake. According to a 2015 national survey, only 64% of providers routinely discussed nutrition with their IBD patients, and less than half reported adequate access to nutrition resources. We aimed to assess provider knowledge, practices, and comfort providing nutrition care to IBD patients across various groups of providers.
Methods: An anonymous 30-question survey was distributed to adult and pediatric gastroenterologists, fellows, and advanced practice providers (APPs) at an academic medical center and its private affiliates. Questions were organized into several domains, including malnutrition knowledge, perceived importance of nutrition, assessment practices, and education and resources. Data were analyzed using descriptive statistics.
Results: 59 providers completed the survey, including 21(36%) IBD-focused attendings (whose practice is ≥ 25% IBD), 17(29%) attendings with IBD experience (whose practice < 25% IBD), 14(24%) fellows, and 7(12%) APPs. 47% of providers had a strong knowledge base surrounding malnutrition in IBD (answered ≥ 3/5 knowledge-based questions correctly), with the largest gaps in recognizing clinical features of malnutrition and micronutrient testing. 91% of providers found nutrition care important in the overall management of IBD patients and identified their role in assessing nutrition risk. Despite this, 53% of providers (47% of adult providers; 88% of pediatric providers) routinely provide nutrition counseling, citing barriers of insufficient time and limited knowledge. 98% of providers stated they would benefit from additional education about nutrition, preferably in the form of lectures (88%) and web-based materials (56%), with 88% requesting standardized patient-facing handouts.
Discussion: While most providers recognized the risk of malnutrition in IBD patients and agreed that identifying and treating malnutrition is within their role, there were considerable gaps in reported nutrition assessments. Less than half of adult providers routinely offer nutrition counseling due to limited time and knowledge, with self-reported limitations underestimating even larger gaps in malnutrition knowledge. Significant work is needed to improve provider education and expand patient-directed resources to standardize and advance nutrition care for IBD patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Emily Gore indicated no relevant financial relationships.
Brijen Shah indicated no relevant financial relationships.
Stephanie Gold indicated no relevant financial relationships.
Emily Gore, MD, Brijen Shah, MD, Stephanie Gold, MD. P4316 - Provider Perceptions and Practices Related to Nutrition Care in Patients with Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
