Tuesday Poster Session
Category: IBD
P4324 - Following a Stricter Diet Is Associated With Higher Confidence in Managing IBD But Also a Higher Perceived Diet Burden
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jamie Horrigan, MD
Dartmouth Hitchcock Medical Center
Lebanon, NH
Presenting Author(s)
Jamie Horrigan, MD1, Jessica Salwen-Deremer, PhD1, Corey A.. Siegel, MD, MS2
1Dartmouth Hitchcock Medical Center, Lebanon, NH; 2Dartmouth-Hitchcock Medical Center, Lebanon, NH
Introduction: Many patients with inflammatory bowel disease (IBD) use diet to manage symptoms and potentially improve inflammation. Our aims were to define a spectrum in patients’ dietary preferences or “dietypes” and to understand how a stricter diet may be associated with other factors.
Methods: We ran four focus groups of 5-6 participants with IBD to learn about their dietary preferences and aimed to develop either specific “dietype” categories or a spectrum of “dietypes.” Focus groups were repeated until thematic saturation was achieved. We then developed a questionnaire targeting adults with IBD on social media to learn more about their dietary preferences and the burden of these preferences.
Results: Demographics of participants are shown in Table 1. 60% reported currently following a special diet, 34% previously followed a special diet, and 6% had never tried a special diet to help manage their IBD. 80% believe that diet has an impact on their IBD. The most common current special diets include avoiding trigger foods (47.3%), gluten and dairy free (12.6%), gluten free (12.6%), dairy free (9%), low fiber/low residue (7.6%), and Mediterranean diet (5.1%) . Other diets including Specific Carbohydrate Diet, low FODMAP, paleo, and ketogenic diets had < 5% following each (n=277).
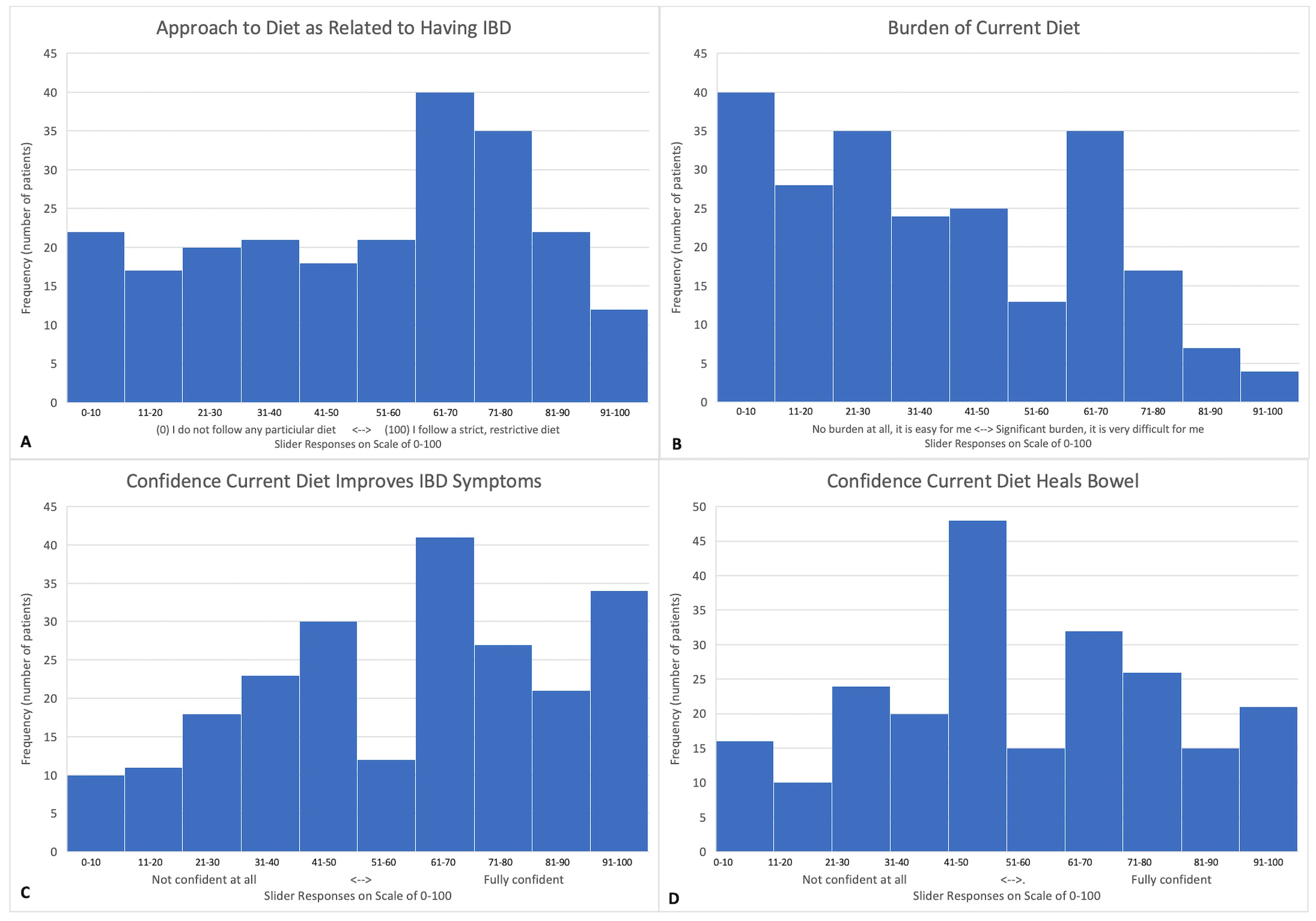
There was wide variation in perceived strictness of current diets. Most viewed their diets as not a major burden and were confident that their diet improves their symptoms but unsure if diet was helping to heal their bowel (Figure 1).
Increased strictness of current diet positively correlated with confidence in control and management of health problems related to IBD (r=0.20, p=0.04). There was also a positive relationship between perceived strictness of current diet and burden of current diet (r=0.38, p< 0.001). Higher PHQ4 (measuring anxious and depressive symptoms) scores correlated with increased perceived burden of current diet (r=0.32, p< 0.001). Similarly, increased perceived burden of diet correlated with increasing severity of ARFID symptoms (r= 0.43, p< 0.001).
Discussion: Most respondents use dietary therapy to help manage their IBD. While following a stricter diet is associated with having more control over their disease, it is also associated with a higher perceived burden, and higher burden is associated with increased symptoms of anxiety, depression, and ARFID. It is important to help patients find a dietype that improves their confidence in managing their disease without creating psychosocial consequences.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jamie Horrigan, MD1, Jessica Salwen-Deremer, PhD1, Corey A.. Siegel, MD, MS2. P4324 - Following a Stricter Diet Is Associated With Higher Confidence in Managing IBD But Also a Higher Perceived Diet Burden, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Dartmouth Hitchcock Medical Center, Lebanon, NH; 2Dartmouth-Hitchcock Medical Center, Lebanon, NH
Introduction: Many patients with inflammatory bowel disease (IBD) use diet to manage symptoms and potentially improve inflammation. Our aims were to define a spectrum in patients’ dietary preferences or “dietypes” and to understand how a stricter diet may be associated with other factors.
Methods: We ran four focus groups of 5-6 participants with IBD to learn about their dietary preferences and aimed to develop either specific “dietype” categories or a spectrum of “dietypes.” Focus groups were repeated until thematic saturation was achieved. We then developed a questionnaire targeting adults with IBD on social media to learn more about their dietary preferences and the burden of these preferences.
Results: Demographics of participants are shown in Table 1. 60% reported currently following a special diet, 34% previously followed a special diet, and 6% had never tried a special diet to help manage their IBD. 80% believe that diet has an impact on their IBD. The most common current special diets include avoiding trigger foods (47.3%), gluten and dairy free (12.6%), gluten free (12.6%), dairy free (9%), low fiber/low residue (7.6%), and Mediterranean diet (5.1%) . Other diets including Specific Carbohydrate Diet, low FODMAP, paleo, and ketogenic diets had < 5% following each (n=277).
There was wide variation in perceived strictness of current diets. Most viewed their diets as not a major burden and were confident that their diet improves their symptoms but unsure if diet was helping to heal their bowel (Figure 1).
Increased strictness of current diet positively correlated with confidence in control and management of health problems related to IBD (r=0.20, p=0.04). There was also a positive relationship between perceived strictness of current diet and burden of current diet (r=0.38, p< 0.001). Higher PHQ4 (measuring anxious and depressive symptoms) scores correlated with increased perceived burden of current diet (r=0.32, p< 0.001). Similarly, increased perceived burden of diet correlated with increasing severity of ARFID symptoms (r= 0.43, p< 0.001).
Discussion: Most respondents use dietary therapy to help manage their IBD. While following a stricter diet is associated with having more control over their disease, it is also associated with a higher perceived burden, and higher burden is associated with increased symptoms of anxiety, depression, and ARFID. It is important to help patients find a dietype that improves their confidence in managing their disease without creating psychosocial consequences.
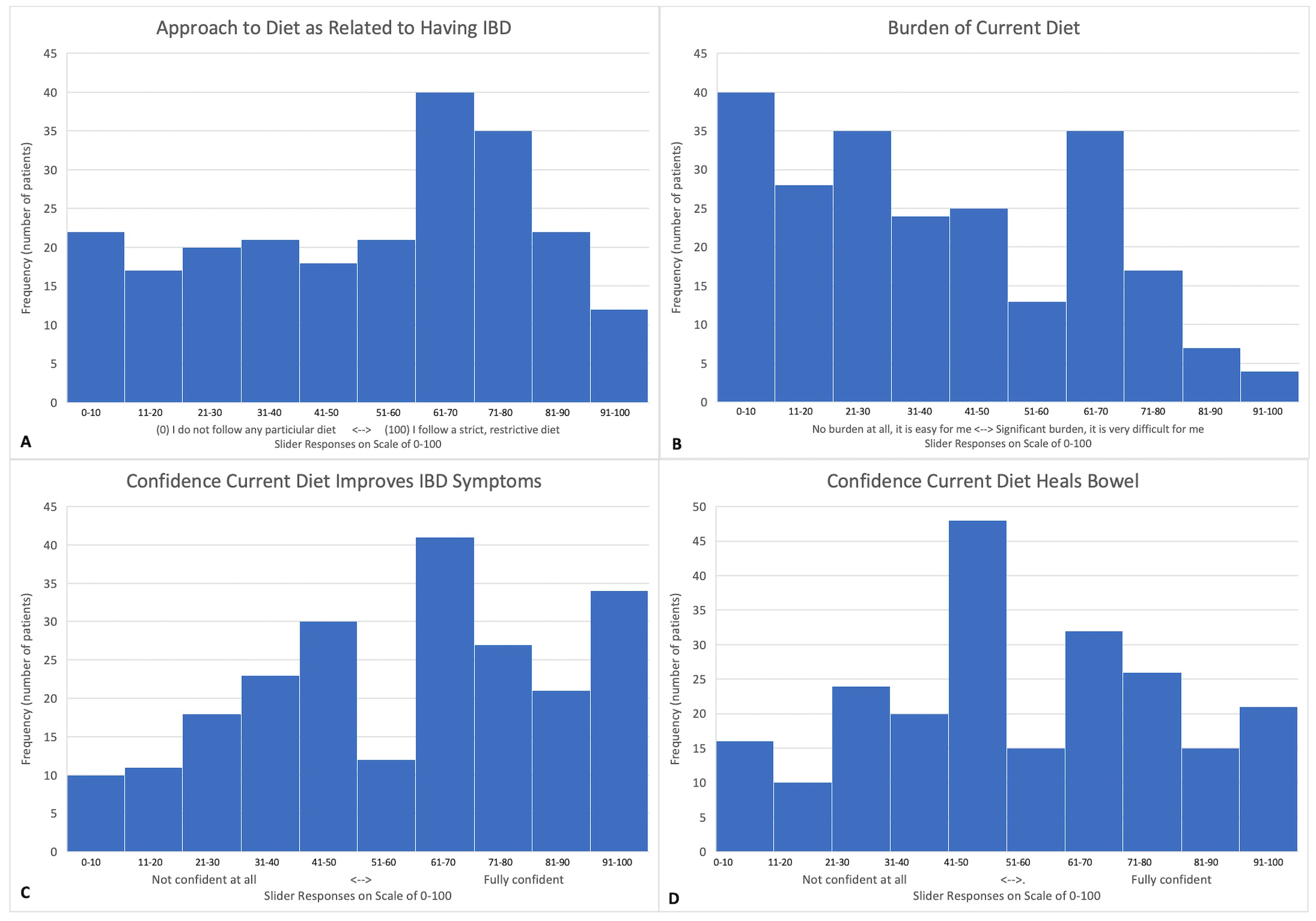
Figure: Figure 1. Patients with inflammatory bowel disease (IBD) were asked to place the slider on a scale from 0 to 100 where it best represented their (A) approach to diet as related to having IBD from “0” “I do not follow any particular diet” to “100” “I follow a strict restrictive diet” (n=228), (B) burden of their current diet from “0” “No burden at all, it is easy for me” to “100” “Significant burden, it is very difficult for me” (n=228), (C) confidence their current diet improves their IBD symptoms from “0” “Not confident at all, I do not think the diet I am currently following improves my IBD symptoms” to “100” “Fully confident, I strongly believe the diet I am currently following improves my IBD symptoms” (n=227), and (D) confidence their current diet heals their bowel from “0” “Not confident at all, I do not think the diet I am currently following helps heal my bowel due to my IBD” to “100” “Fully confident, I strongly believe the diet I am currently following helps heal my bowel due to my IBD” (n=227).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jamie Horrigan indicated no relevant financial relationships.
Jessica Salwen-Deremer indicated no relevant financial relationships.
Corey Siegel: Abbvie – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker for CME activities. BMS – Advisory Committee/Board Member, Consultant. Boomerang – Advisory Committee/Board Member, Consultant. Buhlman – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker for CME activities. Lilly – Advisory Committee/Board Member, Consultant. Napo pharmaceuticals – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support, speaker for CME activities. Prometheus Biosciences – Advisory Committee/Board Member, Consultant. Prometheus Labs – Advisory Committee/Board Member, Consultant. Roivant – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, speaker for CME activities. Trellus Health – Advisory Committee/Board Member, Consultant.
Jamie Horrigan, MD1, Jessica Salwen-Deremer, PhD1, Corey A.. Siegel, MD, MS2. P4324 - Following a Stricter Diet Is Associated With Higher Confidence in Managing IBD But Also a Higher Perceived Diet Burden, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
