Tuesday Poster Session
Category: IBD
P4365 - Is Metabolic Syndrome a Common Comorbidity in Patients With Inflammatory Bowel Disease? A National Database Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ryan Njeim, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Ryan Njeim, MD1, Sai Shanmukha Sreeram Pannala, MD1, Peter Khouri, MD2, Liliane Deeb, MD1
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2SUNY Downstate Health Sciences University, Staten Island, NY
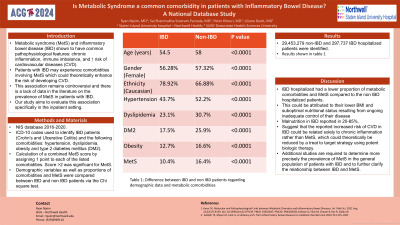
Introduction: Metabolic syndrome (MetS) and inflammatory bowel disease (IBD) have been shown to have common pathophysiological features such as chronic inflammation, immune imbalance, and increased risk of cardiovascular diseases (CVD). IBD patients may experience comorbidities involving MetS which could theoretically enhance the risk of developing CVD. However, this association remains controversial and there is a lack of data in the literature on the prevalence of MetS in IBD patients. Our study aims to evaluate this association specifically in the inpatient setting.
Methods: We included adult patients ( >18 years) in the National Inpatient Sample database between 2016 and 2020. ICD-10 codes were used to identify IBD patients (Crohn’s and Ulcerative Colitis) and the following comorbidities: hypertension (HTN), dyslipidemia, obesity and type 2 diabetes mellitus (DM2). We calculated a combined MetS score by assigning 1 point to each of the listed comorbidities. Score >2 was significant for MetS. Demographic variables as well as proportions of comorbidities and MetS were compared between IBD and non IBD patients via the Chi square test (SAS 9.4 software).
Results: 29,453,279 non-IBD and 297,737 IBD hospitalized patients were identified. Patients in the IBD group were younger when compared to non IBD controls (54.5 vs 58 years, p< 0.0001), and were more often Caucasians (78.92% vs 66.88%, p< 0.0001). In addition, IBD patients had lower proportions of HTN (43.7% vs 52.2%, p< 0.0001), obesity (12.7% vs 16.6%, p< 0.0001), dyslipidemia (23.1% vs 30.7%, p< 0.0001), DM2 (17.5% vs 25.9%, p< 0.0001), and MetS (10.4% vs 16.4%) compared to non IBD patients.
Discussion: We concluded that hospitalized patients with IBD had a lower proportion of metabolic comorbidities and MetS compared to the hospitalized non IBD patients. This could be attributed to their lower body mass index and suboptimal nutritional status resulting from ongoing inadequate control of their disease. In fact, malnutrition has been reported in IBD at rates ranging from 20 to 85%. This finding may suggest that the reported increased risk of CVD in IBD could be related solely to chronic inflammation rather than MetS, which could theoretically be reduced by a treat to target strategy using potent biologic therapy. Additional studies are required to determine more precisely the prevalence of MetS in the general population of patients with IBD and to further clarify the relationship between IBD and MetS.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ryan Njeim, MD1, Sai Shanmukha Sreeram Pannala, MD1, Peter Khouri, MD2, Liliane Deeb, MD1. P4365 - Is Metabolic Syndrome a Common Comorbidity in Patients With Inflammatory Bowel Disease? A National Database Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2SUNY Downstate Health Sciences University, Staten Island, NY
Introduction: Metabolic syndrome (MetS) and inflammatory bowel disease (IBD) have been shown to have common pathophysiological features such as chronic inflammation, immune imbalance, and increased risk of cardiovascular diseases (CVD). IBD patients may experience comorbidities involving MetS which could theoretically enhance the risk of developing CVD. However, this association remains controversial and there is a lack of data in the literature on the prevalence of MetS in IBD patients. Our study aims to evaluate this association specifically in the inpatient setting.
Methods: We included adult patients ( >18 years) in the National Inpatient Sample database between 2016 and 2020. ICD-10 codes were used to identify IBD patients (Crohn’s and Ulcerative Colitis) and the following comorbidities: hypertension (HTN), dyslipidemia, obesity and type 2 diabetes mellitus (DM2). We calculated a combined MetS score by assigning 1 point to each of the listed comorbidities. Score >2 was significant for MetS. Demographic variables as well as proportions of comorbidities and MetS were compared between IBD and non IBD patients via the Chi square test (SAS 9.4 software).
Results: 29,453,279 non-IBD and 297,737 IBD hospitalized patients were identified. Patients in the IBD group were younger when compared to non IBD controls (54.5 vs 58 years, p< 0.0001), and were more often Caucasians (78.92% vs 66.88%, p< 0.0001). In addition, IBD patients had lower proportions of HTN (43.7% vs 52.2%, p< 0.0001), obesity (12.7% vs 16.6%, p< 0.0001), dyslipidemia (23.1% vs 30.7%, p< 0.0001), DM2 (17.5% vs 25.9%, p< 0.0001), and MetS (10.4% vs 16.4%) compared to non IBD patients.
Discussion: We concluded that hospitalized patients with IBD had a lower proportion of metabolic comorbidities and MetS compared to the hospitalized non IBD patients. This could be attributed to their lower body mass index and suboptimal nutritional status resulting from ongoing inadequate control of their disease. In fact, malnutrition has been reported in IBD at rates ranging from 20 to 85%. This finding may suggest that the reported increased risk of CVD in IBD could be related solely to chronic inflammation rather than MetS, which could theoretically be reduced by a treat to target strategy using potent biologic therapy. Additional studies are required to determine more precisely the prevalence of MetS in the general population of patients with IBD and to further clarify the relationship between IBD and MetS.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ryan Njeim indicated no relevant financial relationships.
Sai Shanmukha Sreeram Pannala indicated no relevant financial relationships.
Peter Khouri indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Ryan Njeim, MD1, Sai Shanmukha Sreeram Pannala, MD1, Peter Khouri, MD2, Liliane Deeb, MD1. P4365 - Is Metabolic Syndrome a Common Comorbidity in Patients With Inflammatory Bowel Disease? A National Database Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
