Tuesday Poster Session
Category: IBD
P4366 - Biologic Therapy and Proton Pump Inhibitors in Inflammatory Bowel Disease: Impact on Clostridium difficile Infection Risk
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ryan Njeim, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Ryan Njeim, MD, Reem Dimachkie, MD, Chapman Wei, MD, Liliane Deeb, MD
Staten Island University Hospital, Northwell Health, Staten Island, NY
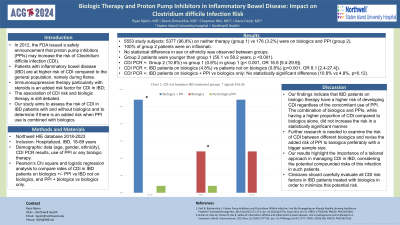
Introduction: In 2012, the FDA issued a safety report that proton pump inhibitors (PPIs) may increase the risk of Clostridium difficile infection (CDI). Additionally, it is established that patients with inflammatory bowel disease (IBD) are at higher risk of CDI compared to the general population, namely during flares. Immunosuppressive therapy particularly with steroids is an added risk factor for CDI in IBD; however, whether biologic therapy is associated with a higher risk of CDI is still debated. Thus, our study aims to assess the risk of CDI in IBD patients with and without biologics and to determine if there is an added risk when PPI use is combined with biologics.
Methods: Using Northwell HIE database 2018-2023, we included adult hospitalized IBD patients, checking their age, sex, ethnicity, CDI PCR results, use of PPI or any biologic therapy. Using the Chi square test and logistic regression analysis, we compared the CDI rates in IBD patients on biologics with and without PPI to IBD patients not on biologics. We also compared patients on both PPI and biologics to patients on biologics only.
Results: 5377 (96.8%) IBD patients were on neither therapy (group 1) and 176 (3.2%) were on biologics and PPI (group 2). No statistical difference in sex or ethnicity was observed between groups. Group 2 patients were younger than group 1 (50.1 vs 58.2 years, p < 0.001). CDI PCR was positive in 10.8% of patients in group 2 vs 0.8% in group 1 (p< 0.001, OR 16.8 [9.4-29.9]). Comparing IBD patients on biologics to patients not on biologics, CDI rates were 4.8% in the former vs 0.8% in the latter (p< 0.001, OR 8.1 [2.4-27.4]). However, comparing patients on biologics and PPI to patients on biologics only did not show a statistically significant difference (10.8% vs 4.8%, p=0.12).
Discussion: Our findings indicate that IBD patients on biologic therapy have a higher risk of developing CDI regardless of the concomitant use of PPI. The combination of biologics and PPIs, while having a higher CDI rate compared to biologics alone, did not increase the risk significantly. Further research is needed to examine the risk of CDI between different biologics and revise the added risk of PPI to biologics preferably with a bigger sample size. Our results highlight the importance of a tailored approach in managing CDI in IBD, considering the potential compounded risks of this infection in such patients. Clinicians should carefully evaluate all CDI risk factors in IBD patients treated with biologics to minimize this risk.
Disclosures:
Ryan Njeim, MD, Reem Dimachkie, MD, Chapman Wei, MD, Liliane Deeb, MD. P4366 - Biologic Therapy and Proton Pump Inhibitors in Inflammatory Bowel Disease: Impact on <i>Clostridium difficile</i> Infection Risk, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: In 2012, the FDA issued a safety report that proton pump inhibitors (PPIs) may increase the risk of Clostridium difficile infection (CDI). Additionally, it is established that patients with inflammatory bowel disease (IBD) are at higher risk of CDI compared to the general population, namely during flares. Immunosuppressive therapy particularly with steroids is an added risk factor for CDI in IBD; however, whether biologic therapy is associated with a higher risk of CDI is still debated. Thus, our study aims to assess the risk of CDI in IBD patients with and without biologics and to determine if there is an added risk when PPI use is combined with biologics.
Methods: Using Northwell HIE database 2018-2023, we included adult hospitalized IBD patients, checking their age, sex, ethnicity, CDI PCR results, use of PPI or any biologic therapy. Using the Chi square test and logistic regression analysis, we compared the CDI rates in IBD patients on biologics with and without PPI to IBD patients not on biologics. We also compared patients on both PPI and biologics to patients on biologics only.
Results: 5377 (96.8%) IBD patients were on neither therapy (group 1) and 176 (3.2%) were on biologics and PPI (group 2). No statistical difference in sex or ethnicity was observed between groups. Group 2 patients were younger than group 1 (50.1 vs 58.2 years, p < 0.001). CDI PCR was positive in 10.8% of patients in group 2 vs 0.8% in group 1 (p< 0.001, OR 16.8 [9.4-29.9]). Comparing IBD patients on biologics to patients not on biologics, CDI rates were 4.8% in the former vs 0.8% in the latter (p< 0.001, OR 8.1 [2.4-27.4]). However, comparing patients on biologics and PPI to patients on biologics only did not show a statistically significant difference (10.8% vs 4.8%, p=0.12).
Discussion: Our findings indicate that IBD patients on biologic therapy have a higher risk of developing CDI regardless of the concomitant use of PPI. The combination of biologics and PPIs, while having a higher CDI rate compared to biologics alone, did not increase the risk significantly. Further research is needed to examine the risk of CDI between different biologics and revise the added risk of PPI to biologics preferably with a bigger sample size. Our results highlight the importance of a tailored approach in managing CDI in IBD, considering the potential compounded risks of this infection in such patients. Clinicians should carefully evaluate all CDI risk factors in IBD patients treated with biologics to minimize this risk.
Disclosures:
Ryan Njeim indicated no relevant financial relationships.
Reem Dimachkie indicated no relevant financial relationships.
Chapman Wei indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Ryan Njeim, MD, Reem Dimachkie, MD, Chapman Wei, MD, Liliane Deeb, MD. P4366 - Biologic Therapy and Proton Pump Inhibitors in Inflammatory Bowel Disease: Impact on <i>Clostridium difficile</i> Infection Risk, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
